Plavix
Plavix
Plavix dosages: 75 mg
Plavix packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
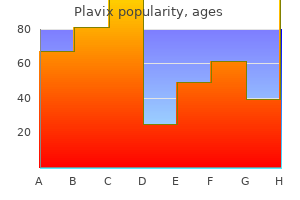
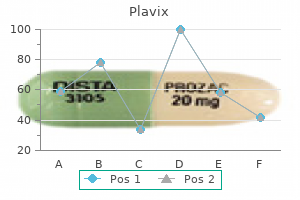
The interosseous border is sharp pulse pressure greater than 40 discount plavix 75 mg fast delivery, besides proximally blood pressure medication low blood pressure quality plavix 75 mg, close to the tuberosity arrhythmia questionnaire discount plavix 75 mg without prescription, and distally, the place the interosseous border is the posterior margin of a small, elongated, triangular area, proximal to the ulnar notch. The interosseous membrane is connected to the distal three-quarters of the radial shaft, and connects the radius to the ulna. The anterior surface, between anterior and interosseous borders, is concave transversely and shows a distal anterior curvature. There is a proximally directed nutrient foramen and canal close to the midpoint of the shaft. The posterior surface of the shaft, between the interosseous and posterior borders, is essentially flat but may be barely hollow proximally. A finely irregular oval space happens near the midshaft; further distally, the surface is easy. The lateral floor is slightly tough, projecting distally as the radial styloid process. The smooth carpal articular floor is split by a ridge into medial and lateral areas. The medial distal radial articular surface is quadrangular, whereas the lateral a half of the articular surface is triangular and curves on to the styloid process. The anterior floor of the distal radius is a thick, palpable, outstanding ridge 2 cm the proximal articular surface of the radial head and its circumference are lined by hyaline cartilage. The upper rim matches the groove between the capitulum and trochlea and enters the radial fossa in flexion. The articular circumference articulates with the ulnar radial notch and anular ligament, within which it rotates in pronation and supination. The posterior area of the tuberosity is marked by the tendon of biceps brachii, which is separated from a easy anterior area by a bursa. Flexor digitorum superficialis is attached to the proximal anterior floor of the radius by a skinny, broad head. Flexor pollicis longus has an in depth attachment to the proximal two-thirds of the anterior surface of the radial shaft, overlying the nutrient foramen. Pronator quadratus is connected to the distal quarter of the anterior radial shaft; a small, triangular space proximal to the ulnar notch gives attachment to the deepest a half of the muscle. Pronator teres is attached to a tough area near the midpoint of the lateral floor of the radial shaft, at its maximal curvature. Proximally, supinator is hooked up to an extended, V-shaped area on the lateral floor of the shaft. Key: 1, triceps; 2, biceps; three, supinator; 4, abductor pollicis longus; 5, pronator teres; 6, extensor pollicis brevis; 7, subcutaneous space; eight, anconeus; 9, posterior border: attachment for frequent aponeurosis of extensor carpi ulnaris, flexor carpi ulnaris, flexor digitorum profundus; 10, extensor pollicis longus; eleven, extensor indicis. Key: 1, styloid strategy of radius; 2, dorsal tubercle; 3, groove for tendon of extensor carpi ulnaris; four, styloid strategy of ulna; 5, side for scaphoid; 6, facet for lunate; 7, inferior radio-ulnar articulation; 8, area of contact with articular disc; 9, area for attachment of articular disc. On the posterior floor, abductor pollicis longus is hooked up proximally, and extensor pollicis brevis more distally. The remaining floor is devoid of attachments and lined by the lengthy and quick extensors of the thumb. The lateral floor, proximal to the styloid process, receives the attachment of brachioradialis and is crossed obliquely, downwards and forwards, by the tendons of abductor pollicis longus and extensor pollicis brevis. The radial styloid course of tasks beyond that of the ulna, its apex lined by the tendons of abductor pollicis longus and extensor pollicis brevis. The lateral radiocarpal ligament is attached to its tip, and the palmar radiocarpal ligament is hooked up to the terminal ridge on the anterior surface of the lower finish. The base of the triangular articular disc of the inferior radio-ulnar joint is connected to a clean ridge distal to the ulnar notch. A slender protrusion of synovial membrane extends proximally from the ulnar notch, anterior to the lower end of the interosseous membrane. The lateral part of the carpal articular floor articulates with the scaphoid, and the medial half with the lateral part of the lunate. In full adduction, the proximal surface of the lunate is wholly involved with the radius. The radial dorsal tubercle receives a slip from the extensor retinaculum and is grooved medially by the tendon of extensor pollicis longus. The wide groove lateral to the tubercle contains the tendons of extensor carpi radialis longus laterally and extensor carpi radialis brevis medially, together with their synovial sheaths. Medially, the dorsal floor is grooved by the tendons of extensor digitorum, separated from the bone by the tendons of extensor indicis and the posterior interosseous nerve. A network of small fascioperiosteal and musculoperiosteal vessels come up from the compartmental vessels and reach the bone by way of its septal and muscular attachments. Branches connect the anterior interosseous artery proximally to the dorsal carpal arch distally. These pass via the fourth and fifth extensor compartments of the wrist and supply metaphysial nutrient arteries. Intercompartmental vessels send nutrient arteries to the radius via the retinaculum between the first and second dorsal compartments, and the second and third dorsal compartments. These vessels originate from the radial artery and anterior interosseous arteries, respectively, and anastomose with the dorsal carpal arch. Ossification begins in the distal epiphysis in path of the end of the primary postnatal 12 months and in the proximal epiphysis during the fourth 12 months in females and the fifth 12 months in males. A fourth centre generally seems in the tuberosity at about the fourteenth or fifteenth year. The bone diminishes progressively from its proximal mass all through almost its complete length, but, at its distal finish, expands into a small, rounded head and styloid course of. The shaft is triangular in cross-section proximally, and virtually cylindrical distally. Its base is slightly constricted where it joins the shaft and is the narrowest part of the proximal ulna. On the lateral surface, distal to the trochlear notch, a shallow, easy, oval radial notch articulates with the radial head. Distal to the radial notch, the surface is hollow to accommodate the radial tuberosity during pronation and supination. Its distal part is the tuberosity of the ulna and its medial border is sharp and bears a small tubercle proximally. It is constricted on the junction of the olecranon and coronoid processes, the place their articular surfaces could also be separated by a slender, tough, non-articular strip. A easy ridge, adapted to the groove on the humeral trochlea, divides the notch into medial and lateral parts. The radial notch, an oval or oblong proximal despair on the lateral aspect of the coronoid course of, articulates with the periphery of the radial head and is separated from the trochlear notch by a smooth ridge. Proximal ulna the proximal finish of the ulna has large olecranon and coronoid processes, and trochlear and radial notches that articulate with the humerus and radius, respectively. The olecranon is more proximal and is bent forwards at its summit like a beak that enters the olecranon fossa of the humerus in extension. In extension, it could be felt near a line joining the humeral epicondyles, but in flexion, it descends, in order that the three osseous points kind an isosceles triangle. It has anterior, posterior and medial surfaces and interosseous, posterior and anterior borders. Proximally, it becomes the supinator crest, which is steady with the posterior border of a despair distal to the radial notch. The rounded anterior border starts medial to the ulnar tuberosity, descends backwards, and is normally traceable to the base of the styloid process. It is palpable all through its length in a longitudinal furrow, most evident when the elbow is absolutely flexed. Proximal to its midpoint, a proximally directed nutrient foramen admits a department of the anterior interosseous artery. The medial floor, between the anterior and posterior borders, is transversely convex and easy. The posterior floor, between the posterior and interosseous borders, is split into three areas. The most proximal is limited by a sometimes faint, oblique line that ascends laterally from the junction of the middle and upper thirds of the posterior border to the posterior end of the radial notch. The region distal to this line is split into a bigger medial and narrower lateral strip by a vertical ridge, which is usually distinct solely in its proximal three-quarters.
Second rib the second rib is twice the length of the primary and has a similar curvature heart attack 27 plavix 75 mg order overnight delivery. The exterior floor of the shaft is convex and superolaterally is marked centrally by a rough blood pressure ranges by age and gender cheap plavix 75 mg visa, muscular impression that continues posteromedially towards the tubercle as a slender blood pressure medication reviews discount plavix 75 mg, roughened ridge. The distinct lips of the higher border are widely separated behind; scalenus posterior and serratus posterior superior are attached to the outer lip in entrance of the angle. These attachments vary: these of the inner intercostal, levator costae and erector spinae merge and people of latissimus dorsi, diaphragm and exterior oblique may reach the costal cartilage. Its lateral finish is normally below the road of costodiaphragmatic pleural reflection and is therefore not lined by pleura. Vascular provide and innervation the blood supply of the second rib is by way of the interior thoracic and superior intercostal arteries. Venous drainage is via the superior intercostal vein, which drains into the brachiocephalic vein, and the anterior intercostal veins, which drain into the inner thoracic vein. Ossification the second rib is ossified from a main centre for the shaft, which seems close to the angle late within the second month. The secondary centres for the top and articular and non-articular components of the tubercle seem about puberty, uniting to the shaft quickly after the age of 20 years. Vascular provide and innervation the tenth and eleventh ribs are equipped by the posterior intercostal artery and branches from the musculophrenic artery. Venous drainage is by way of the posterior intercostal and subcostal veins, which in turn drain into the azygos system. There is extra drainage via the anterior intercostal veins (branches of the musculophrenic vein). The tenth and eleventh ribs are innervated by the corresponding intercostal nerve, and the twelfth rib is innervated by the subcostal nerve. Ossification the tenth rib ossifies from a primary centre in the shaft and secondary centres for the head and articular components of the tubercle. Tenth, eleventh and twelfth ribs the tenth rib has a single aspect on its head that may articulate with the intervertebral disc above, in addition to the upper border of the tenth thoracic vertebra near its pedicle. The eleventh and twelfth ribs every have one giant articular aspect on the pinnacle but no neck or tubercle. The twelfth rib has neither, is way shorter and slopes cranially at its vertebral end. Quadratus lumborum and its anterior covering layer of thoracolumbar fascia are attached to the lower a half of its anterior surface in its medial one-half to two-thirds; the upper part is expounded to the costodiaphragmatic pleural recess. The inner intercostal muscle (medially) and the diaphragm (laterally) are attached at or near the upper border. The decrease border gives attachment to the center lamella of the thoracolumbar fascia and, lateral to quadratus lumborum, to the lateral arcuate ligament and posterior lamella of the thoracolumbar fascia. The lumbocostal ligament is connected posteriorly, close to the head, connecting it to the primary lumbar transverse course of. The lowest Costal cartilages Costal cartilages are the persistent, ossified anterior elements of the cartilaginous models during which the ribs develop. The upper seven pairs be part of the sternum; the eighth to tenth articulate with the lower border of the cartilage above; and the lowest two have free, pointed ends within the stomach wall. They increase in length from the primary to the seventh, after which decrease to the twelfth. The costal cartilages are broad at their costal continuity and taper as they cross forwards. The first and second are of even breadth and the sixth to eighth enlarge where their margins are involved. The first descends a little, the second is horizontal and the third ascends barely; the others are angulated and incline up in course of the sternum or cartilage above, somewhat anterior to their ribs. The sternoclavicular articular disc, costoclavicular ligament and subclavius are connected to the primary costal cartilage. Pectoralis main is hooked up to the medial aspect of the first six cartilages and the others are covered by the partial attachments of the anterior belly muscle tissue. Key: 1, attachment of internal intercostal muscle; 2, attachment of costotransverse ligament; three, head; 4, area coated by pleura; 5, attachment of diaphragm; 6, line of pleural 5 reflection; 7, attachment of quadratus lumborum. Key: 1, attachment of latissimus dorsi; 2, attachment of external oblique; 3, attachment of serratus posterior inferior; four, attachment of exterior intercostal muscle; 6 5, attachment of levator costae; 6, head; 7 7, attachment of erector spinae. The internal intercostal muscles and external intercostal membranes are hooked up to the concave superior and convex inferior borders. The inferior borders of the fifth (sometimes) and sixth to ninth cartilages project at points of greatest convexity. Oblong facets on these projections articulate with aspects on slight projections from the superior borders of subjacent cartilages. The medial finish of the primary is continuous with the sternum; these of the six succeeding cartilages are spherical and articulate with shallow costal notches on the lateral margins of the sternum; these of the eighth to tenth are pointed, every connected with the cartilage above; and people of the eleventh and twelfth are pointed and free. With the exception of the fibrous synarthrosis between the first rib and sternum, all these articulations are synovial. Despite their pliability, the ribs are rather more frequently damaged, the middle ribs being essentially the most vulnerable. Because traumatic stress is usually the outcomes of compression of the thorax, the identical old website of fracture is simply in front of the angle, which is the weakest level of the rib. Direct impact might fracture a rib at any point; the ends of the broken bone may be driven inwards and doubtlessly could injure thoracic or upper stomach viscera. The bony surfaces are covered by hyaline cartilage and connected by a fibrocartilage, which may ossify within the aged. Sometimes, the central a half of the disc is absorbed and the joint appears synovial. The manubriosternal joint is linked by a fibrous membrane enveloping the complete bone. In occasional people over the age of 30 years, the manubrium is joined to the sternal body by bone but the intervening cartilage could also be only superficially ossified; ossification turns into full only within the aged. Early synostosis has been attributed to a persistent synchondrosis in place of a symphysis. The first and tenth to twelfth ribs articulate with a single vertebra by a easy synovial joint. In the others, an intra-articular ligament bisects the joint, producing a double synovial compartment, so the joint is classed as each compound and sophisticated. Often inaccurately described as aircraft, their articular surfaces are barely ovoid and the upper and decrease synovial articulations are obtusely angled to each other. The powerful ligamentous attachments on this region imply that dislocation of the manubriosternal joint is rare, though it could be associated with high-energy trauma. Dislocation is commonest when the joint is synovial, whereas synchondral and synosteal types usually fracture by way of the manubrium. Fibrous capsules the fibrous capsule connects the costal head to the circumference of the articular surface formed by an intervertebral disc and the demifacets of two adjoining vertebrae. Some of the upper fibres traverse their intervertebral foramina to mix with the posterior aspects of the intervertebral discs. Radiate ligaments Radiate ligaments join the anterior elements of every costal head to the bodies of two vertebrae and their intervening intervertebral disc. Intermediate fibres, shortest and least distinct, are horizontal and hooked up to the disc. The radiate ligament related to the first rib is connected to the seventh cervical and first thoracic vertebrae. In the joints of the tenth to twelfth ribs, which articulate with single vertebrae, the radiate ligament is connected to the numbered vertebra and the one above. It is normally transformed to a synostosis by the fortieth year but sometimes stays unchanged, even in old age. Intra-articular ligament the intra-articular ligament is a brief flat band attached laterally to the crest between the costal articular aspects and medially to the intervertebral disc, dividing the joint. In the upper 5 - 6 joints, articular Chest wall and breast When current, marginal and central subperichondrial ossification patterns seen on X-ray afford a comparatively simple, rapid, inexpensive and accurate means of identifying sex in fully or partially skeletonized and unidentified human materials, offering the topic is over 20 years of age. In males, the predictive capacity of the marginal subperichondrial ossification sample is 75�80%. In females, the predictive capability for a central subperichondrial ossification sample is bigger than 90%. Third thoracic vertebra Accessory ligament An accessory ligament is usually current.
Diseases
Better described as having discordant ventriculo�arterial connections prehypertension at 19 plavix 75 mg generic free shipping, such hearts can coexist with deficiencies of cardiac septation arrhythmia treatment algorithm discount 75 mg plavix amex. They may additionally be found with discordant connections on the atrioventricular junctions blood pressure medication side effects discount plavix 75 mg free shipping, producing congenitally corrected transposition. Double outlet ventricle exists when the greater components of both arterial valves are attached throughout the identical ventricle, virtually at all times the right. It is normally beneath the aorta or the pulmonary trunk, but may be doubly committed or even non-committed. Right and left superior vena cavae are present in some animals and infrequently persist in mankind. The most common systemic anomaly is a persistent left superior vena cava draining into the proper atrium by way of the enlarged orifice of the coronary sinus. The most common lesion of the inferior vena cava is when its stomach course is interrupted, with drainage to the heart via the azygos or hemiazygos venous system. This lesion is discovered most regularly with isomerism of the left atrial appendages. The pulmonary veins can be connected to an anomalous web site individually or in combination. Usually, the veins type a confluence behind the left atrium, which then connects to the superior vena cava, the coronary sinus or the portal venous system after traversing the diaphragm. Neonatal peripheral vessels are nearly microscopic; consequently, their cannulation poses much more of an issue than is the case with their adult counterparts. Large vessels are in the identical relative positions as in the adult however may correspond to different vertebral levels. The renal arteries also arise larger in the neonate, typically between T12 and L1, whereas they come up at the upper border of L2 within the grownup. The belly aorta bifurcates into common iliac arteries on the higher border of L4, quite than on the lower border of L4, as happens in the adult. SeCtIon 7 Central venous catheterization Small-bore catheters can be fed into giant central veins or into the best atrium via needles or catheters inserted in the peripheral veins. Typically, the median cubital or basilic veins are used in the upper limb, the lengthy saphenous vein on the medial malleolus within the lower limb and the superficial temporal vein within the scalp. The required catheter size is assessed from direct measurement of the distance between the purpose of surface entry in the limb to the right atrium, estimated at mid-sternal level. Development of each tree is related to the opposite and all proceed in proximal to distal growth and growth. Uniquely, the lung develops whereas not fulfilling its postnatal perform, and must operate efficiently immediately after start or else the child would require respiratory support and should die of respiratory failure. Current data of the molecular foundation of lung development is predicated on development in vitro of human and animal explants (usually mouse and rat), and research utilizing knockout and transgenic mice (Herriges et al 2012). The reader is referred to latest studies of lung developmental biology for extra data (Roth-Kleiner and Post 2005, Kimura and Deutsch 2007, Maeda et al 2007, Bhaskaran et al 2009, Kho et al 2010, Morrisey and Hogan 2010, Sgantzis et al 2011, Ornitz and Yin 2012). The specialist respiratory epithelium forms from the endoderm, whereas the other elements of the airway wall are of mesenchymal origin. By stage 13, the caudal end of the tube has divided asymmetrically to type the longer term major bronchi; with progress, the proper major bronchus becomes oriented more caudally, whereas the left extends extra transversely. From this time, the origin of the trachea remains close to its web site of evagination from the lengthy run oesophagus; however, longitudinal growth of the trachea causes the region of the long run carina to descend, finally to lie throughout the thorax. Failure of complete separation between trachea and oesophagus will outcome within the child being born with one of the variants of tracheo-oesophageal fistula (see below). The medical counterpart is the observation that preterm males might have worse respiratory misery than females after management for other threat factors, similar to diploma of prematurity. The point at which the original respiratory diverticulum buds from the foregut, the laryngotracheal groove, remains at a continuing stage during the embryonic period, and the trachea lengthens distally because the bifurcation level descends. The respiratory diverticulum generally turns into surrounded by angiogenic mesenchyme that connects to the developing sixth aortic arch artery and is important for airway branching. By stage 17, the mesenchyme across the trachea is beginning to condense to type cartilage. Progressive lengthening and continued division of the tracheal bud, along with deviation of the lung buds dorsally, isolates the oesophagus and trachea inside tissue-specific mesenchyme and facilitates regional differentiation, not only between trachea and lungs, but in addition inside the lungs themselves, i. For branching to occur, a cleft should develop within the tip (or side) of the epithelial tube. At the ideas of the creating epithelial buds, the mesenchyme is flattened and densely packed, whereas it forms an ordered row of cuboidal cells alongside the aspect of the bud and within the clefts. Cells in both preparations ship processes in direction of the epithelial basal lamina, which is thicker in the clefts, but so attenuated as to be nearly indistinguishable on the information of the buds where the epithelium and mesenchymal cells form intimate contacts. Tenascin, an extracellular matrix molecule, is present within the budding and distal tip regions, however absent within the clefts. Conversely, fibronectin, an extracellular Yolk sac matrix molecule found generally in basal laminae, is found within the clefts and along the perimeters of the growing bronchi, but not on the budding and distal suggestions. The control of the branching pattern of the respiratory tree resides with the splanchnopleuric mesenchyme. Experimental recombination of tracheal mesenchyme with bronchial respiratory endoderm ends in inhibition of bronchial branching, whereas recombination of bronchial mesenchyme with tracheal epithelium will induce bronchial outgrowths from the trachea. Experimental exposure of rat fetal airway to chick mesenchyme produces a chick airway branching pattern. Interestingly, even at this early stage, airway smooth muscle is innervated and contractile (Tollet et al 2002). Phasic contraction and rest of airways is important in progress factor release. Smooth muscle and nerves are found exterior the airways at this developmental stage. D, Major epithelial populations within the early embryo from a left dorsolateral view. The pulmonary veins become surrounded by myocardium to the extent of the second bifurcation. The veins themselves expand and are included into the roof of the left atrium; cardiac muscle is, due to this fact, found in the central branches of the pulmonary venous tree (Hislop 2005). The lung buds on all sides of the oesophagus project dorsally into the pericardioperitoneal canals at stage 15. After this stage, the coelomic epithelium on the perimeter of the lung surface follows a differentiation pathway to kind the visceral pleura. Later phases of respiratory growth contain the repeated division of the bronchial tree to form the subsegmental bronchi. Endotracheal intubation within the neonate the insertion of an endotracheal tube is a process that could be required to resuscitate the newborn at start and, subsequently, to allow artificial ventilation. The size of the trachea in the neonate could be as short as three cm in untimely infants, and the gap from T1 to carina ranges from 1. Once in place, the tip of the tube ought to be within the mid-trachea, nicely above the carina. If a shouldered tube is used, only the distal, tapered portion of the tube is inserted past the vocal cords, and the shoulders should prevent the tube being superior too far. Confirmation of right positioning of the endotracheal tube is obtained from a chest X-ray. Previously, it was suggested that the tip of the endotracheal tube should be placed just below the clavicles, at the stage of the first rib or 1�2 cm above the carina. It is now instructed that the body of the first thoracic vertebra (T1) is a extra stable reference point as the goal for the tip of the endotracheal tube. Pseudoglandular phase (5�17 weeks: development of airways and blood vessels to level of acinus) By stage 17 (late sixth to early seventh week), the separation of the lungs from the digestive system is full and the pseudoglandular section of pulmonary improvement, which includes the development of the lower conducting airways and the looks of the acinar structures, can be identified. During this period, just about the complete branching construction of the future bronchial tree is laid down, giving rise to 20 generations. The progress and branching of the endoderm epithelium is managed by the native investing splanchnopleuric mesenchyme. Primitive ciliated cells appear at about week 7, initially within the area of the membranous trachea, and within the cartilaginous region by week 12. Ciliary biology and ciliopathy are an rising focus of research (Bush and Hogg 2012). Nodal cilia are also motile and are answerable for determining organ situs in the growing embryo (Nonaka et al 2002).
A ganglion (an outpouching of the synovial membrane of the gleno humeral joint) could occur immediately behind and above the postero superior corner of the glenoid fossa; this can compress the department of the suprascapular nerve that provides infraspinatus as it courses across the lateral side of the backbone of the scapula beneath the inferior scapular ligament blood pressure bottom number low discount plavix 75 mg line. Decompression of the ganglion and division of the ligament are curative in the early stage of this syndrome pulse pressure less than 30 plavix 75 mg cheap. An intraneural ganglion may arise from the articular department of the suprascapular nerve; muscular ache and atrophy could be anticipated to be extra fast than within the case of the synovial ganglion (Spinner et al 2006) blood pressure practice buy 75 mg plavix mastercard. Key: 1, 1 subscapularis; 2, triceps brachii (medial head); three, coracobrachialis; 4, pronator teres (humeral head); 5, widespread flexor origin; 6, supraspinatus; 7, 2 pectoralis major; 8, latissimus dorsi; 9, teres main; 10, deltoid; eleven, brachialis; 12, brachioradialis; 13, extensor carpi radialis longus; 14, widespread extensor origin. Key: 1, infraspinatus; 2, teres minor; 3, triceps brachii (lateral head); 4, deltoid; 5, brachialis; 6, 3 triceps brachii (medial head); 7, anconeus. Key: 1, head; 2, anatomical neck; 3, surgical neck; four, larger tubercle; 5, 5 lesser tubercle; 6, intertubercular sulcus; 7, shaft. Key: 1, greater tubercle; 2, surgical neck; 3, shaft; four, radial groove; 5, head; 6 6, anatomical neck. The distal end is tailored to the forearm bones at the elbow joint and carries the medial and lateral epicondyles with the articular surfaces for the radius and ulna between them. The shaft of the human (and primate) humerus is comparatively medially rotated with respect to the humeral head, in contrast with quadripedal ancestors; this offers the characteristically greater vary of external rota tion on the glenohumeral joint than that getting in different species. This is reflected within the spiroidal structure of the adult humeral medullary cavity, the association and relationship of the posterior compartment of brachial muscle tissue and the radial nerve, and the disposition to long spiroidal fractures brought on by exterior twisting forces. With the arm by the aspect within the anatomical position, and with the medial and lateral epicondyles in the same (frontal) airplane. It is essential to keep in mind this place of the bone when actions of the arm and forearm are thought of; actions are recorded relative to the trunk (starting within the anatomical position) or relative to the scapula, and it is essential to define which methodology is in use. It contains the long tendon of biceps, its synovial sheath, and an ascending department from the anterior circumflex humeral artery. The rough lateral lip of the groove is marked by the bilaminar tendon of pectoralis major, and its medial lip by the tendon and muscular insertion of teres major. The ground of the groove supplies attachment for a frequent upward extension of the tendon of pectoralis main, and for the tendon of latissimus dorsi extra caudally (Dancker 2013). It can be readily palpated laterally and medially, but the muscular tissues of the anterior and posterior compartments obscure the bone to palpation anteriorly and posteriorly. It has three surfaces and three borders, which are only distinct in the direction of the elbow joint. Surfaces Proximal finish the proximal end of the humerus consists of the head, anatomical neck, and the larger and lesser tubercles. The proximal end of the humerus makes up the upper fifth of the length of the bone. A slight roughness indicates the line of capsular attachment of the shoulder joint, aside from at the intertubercular sulcus, the place the long tendon of biceps brachii emerges. Medially, the capsular attachment diverges from the anatomical neck and descends 1 cm or extra on to the shaft. Lesser tubercle the lesser tubercle is anterior to and just distal to the anatomical neck. It is palpable by way of the thickness of deltoid about three cm below the anterior edge of the acromion. The lateral edge of the lesser tubercle is sharp and forms the medial border of the intertubercular sulcus. The transverse ligament of the shoulder (transverse humeral ligament) is attached to the upper aspect of the lateral margin of the tubercle. Greater tubercle 806 the higher tubercle is probably the most lateral a part of the proximal finish of the humerus and initiatives beyond the lateral border of the acromion. The projecting lateral floor of the tubercle presents quite a few vascular foraminae and is roofed by deltoid, producing the conventional rounded contour of the shoulder. A a part of the subacromial bursa might cover the the posterior floor, between the medial and lateral borders, is broad, flat and convex distally. The medial head of triceps is hooked up to the posterior surface over an elongated triangular area, the apex of which is positioned on the medial part of the bone above the extent of the decrease limit of insertion of teres main. The area widens under and covers the whole floor almost down to the decrease end of the bone. The lateral head of triceps is attached to a ridge, generally tough, that descends obliquely and laterally above the attachment for the medial head. Above triceps, the axillary nerve and the posterior circumflex humeral vessels wind across the bone on the deep floor of deltoid. Below the attachment of the lateral head of triceps, however above the attachment of the medial head, a shallow groove runs from the higher medial facet of the surface downwards and laterally towards the lateral border; it accommodates the radial nerve and its branches, and the profunda brachii vessels. The anterolateral floor is bounded by the anterior and lateral borders, and is clean and featureless in its upper part, which is roofed by deltoid. About, or a little above, the middle of this floor, deltoid is connected to the deltoid tubercle. The nerve perforates the lateral intermuscular septum near the bone at the degree of the junction of the higher threefifths and decrease twofifths of the humerus, and enters the anterior compartment of the arm near the anterolateral floor, between brachialis medially and brachioradialis laterally. Coracobrachialis is attached to a protracted tough strip within the middle third of the medial border, posterior to the brachial neurovascular sheath, which lies in shut relation to the humerus in the middle third of this surface. The humeral head of pronator teres is hooked up to a slim space near the lowest a part of the medial supracondylar ridge; the ridge itself gives attachment to the medial intermuscular septum of the arm. A little below its midpoint, the nutrient foramen, which is directed downwards, opens near the medial border. A hookshaped strategy of bone, the supracondylar process, starting from 2 to 20 mm in length, occasionally projects from the anteromedial floor of the shaft, roughly 5 cm proximal to the medial epicondyle. It is curved downwards and forwards, and its pointed apex is linked to the medial border, simply above the epicondyle, by a fibrous band, to which part of pronator teres is attached. The foramen completed by this fibrous band often transmits the median nerve and brachial artery, however generally encloses solely the nerve, or the nerve plus the ulnar artery (in instances of high division of the brachial artery). Its proximal third forms the lateral lip of the intertubercular sulcus and is roughened for muscular attachments. The succeeding portion can additionally be roughened and forms the anterior limit of the deltoid tubercle; the lower half of the border is smooth and rounded. In its middle and higher thirds, the border is barely discernible, but in a wellmarked bone it can be traced upwards to the posterior surface of the higher tubercle. The limbs of the V are broad; the groove for the radial nerve runs downwards and laterally behind the posterior limb and fades away on the decrease a part of the anterolateral surface. The lateral intermuscular septum is connected to the lateral border, and is a condensation of the fascia over the lower a half of deltoid and the neigh bouring brachialis, forming a septum between the anterior and poste rior muscular compartments. The septum is most evident within the lower threefifths of the arm, and is perforated by the radial nerve and accom panying vessels. Lateral border Fractures of the humeral shaft Humeral shaft fractures are widespread; the sample of the fracture and the displacement of the fragments rely upon the force of injury and on the level at which the bone is broken. The centre for the shaft appears near its middle within the eighth week of intrau terine life, and steadily extends towards the ends. Ossification begins in the head earlier than birth (20%) or in the first 6 months afterwards; the higher tubercle starts to ossify during the first 12 months in females and second 12 months in males; the lesser tubercle begins to ossify at concerning the fifth 12 months. By the sixth yr, the centres for the pinnacle and tubercles have joined to form a single massive epiphysis, hollowed out on its inferior floor to adapt to the conical upper end of the metaphysis. This macroscopic topography offers for mechanical stability within the physis during Fuse at sixth yr Medial border the medial border, although rounded, may be recognized with out diffi culty within the decrease half of the shaft, the place it turns into the medial supra condylar ridge. In its proximal third, the medial border is vague till it broadens out to type a triangular area. In its middle third, the medial border is interrupted by a wide, shallow groove, the radial (spiral) groove that crosses the bone obliquely, passing down wards and forwards from its posterior to its anterior surface. The joint on the left aspect is undamaged and the joint on the best facet is shown in coronal section. The proximal humeral epiphysis fuses with the shaft of the humerus at in regards to the thirteenth or fourteenth yr in females, begin ning on the medial side of the physial line, and between the 4 teenth to sixteenth year in males. Costoclavicular ligament the costoclavicular ligament is like an inverted cone, but brief and flattened.
The umbilical wire varieties all the ventral physique wall between the pericardial bulge and the developing exterior genita lia blood pressure chart low discount 75 mg plavix with visa. It encloses a portion of the extraembryonic coelom heart attack prognosis 75 mg plavix generic mastercard, the umbilical coelom heart attack get me going 75 mg plavix safe, into which midgut loop protrudes. When the midgut loop is abruptly returned to the belly cavity, the extra recognizable umbilical twine forms. The cranial end of the allantois turns into thinned and its lumen partially obliterated, and it types the urachus. The mesenchymal core of the umbilical cord is derived by coalescence from somatopleuric amniotic mesenchyme, splanchnopleuric vitellointestinal (yolk sac) mesen chyme and splanchnopleuric allantoic (connecting stalk) mesenchyme. This may current as a brief segment of vitel line duct hooked up to the original ventral side of the ileum; it may remain connected to the umbilicus as a fistula; or it might remain as a liga mentous attachment to the umbilicus. An umbilical hernia happens when loops of intestine protrude right into a widened umbilical wire at time period. The endoder mal cells of the small intestine proliferate and form a layer some three to four cells thick, with mitotic figures throughout. From 7 weeks, blunt projections of the endoderm have begun to form within the duodenum and proximal jejunum; these are the creating villi, which increase in size till, in the duodenum, the lumen turns into tough to discern. By 9 weeks, the duodenum, jejunum and proximal ileum have villi, and the remaining distal portion of ileum develops villi by 11 weeks. Primitive crypts, epithelial downgrowths into the mesenchyme between the villi, seem between 10 and 12 weeks and equally comply with a craniocaudal development. The absorptive enterocytes have microvilli at their apical borders before 9 weeks. An apical tubular system appears at this time, and is com posed of deep invaginations of the apical plasma membrane and membranebound vesicles and tubules; many lysosomal parts (meconium corpuscles) appear within the apical cytoplasm. These latter options are more developed in the ileum than jejunum, are most distinguished at 16 weeks, and diminish by 21 weeks. C�D, the decrease white arrows related to the midgut indicate the relative actions and rotation of the midgut loop throughout the umbilical coelom, and because it returns to the abdominal cavity. E�F, the lower white arrows related to the midgut indicate the relative movements and rotation of the midgut loop within the umbilical coelom, and as it returns to the stomach cavity. G�H, the approximate disposition in the grownup abdomen of the intestine (G) and the mesenteric roots, showing their lines of attachment and principal contained vessels (H). They are organized as a syncytium between the epithelium and the muscularis mucosae, the place they contribute to the extracellular matrix. They migrate from the crypts to the villous axis in a way similar to enterocytes. It is derived from swallowed amniotic fluid, which contains vernix and cellular debris, salivary, biliary, pancreatic and intestinal secretions, and sloughed enterocytes. As the combination passes alongside the intestine, water and solutes are eliminated and mobile particles and proteins concentrated. Meconium accommodates enzymes from the pancreas and proximal intestine in greater concentrations in preterm than in fullterm infants. At 26�30 weeks, the gut exhibits contractions with out common periodicity; from 30�33 weeks, repetitive groups of normal contractions have been seen in preterm neonates. The movement of the basis of this dorsal mesentery, and the large lengthening of its enteric border to be able to match the longitudinal progress of the intestine tube, mirror the spiralizing of the midgut loop within the umbilical coelom. Fetal gut, from 11 weeks, reveals dipeptidase activity in the colon as well as within the small intestine. There is little direct proof of colonic function within the human fetus and neonate. However, the precise outcomes of mammalian research are being correlated to human studies the place attainable. A variety of distinct and necessary variations between the operate of adult and fetal colon have been reported. Small gut at birth the radial patterning of the small intestine is completed earlier than start, with differentiation of the crypt�villous axis. Specification of the house between villi, crypt depth and villous length is a dynamic process dependent on the institution of the intestinal microbiota. In the neonate, the small gut types an ovalshaped mass with its higher diameter transversely oriented in the abdomen, rather than vertically as in the adult. The mass of the small intestine inferior to the umbilicus is compressed by the urinary bladder, which is anterior at this level. The small intestine is 300�350 cm lengthy at start and its width, when empty, is 1�1. The ratio between the size of the small and the size of the massive intestine at delivery is much like the grownup ratio. The mucosa and submucosa are fairly properly developed and villi are current all through the small gut; however, some epithelial differentiation is incomplete. There are few or no circular folds in the small gut, and the jejunum and ileum have little fats in their mesentery. In the grownup, the presence of bile salts in the colon stimulates the secretion of water and electrolytes, which finally ends up in diarrhoeal syndrome; however, the fetal and neonatal colon appears protected against this impact. Thus, it seems that the colon fulfils a barely different role in the preterm and neonatal period, conserving nutrient absorption and minimizing fluid loss until the neonate has adjusted to extrauterine life, oral feeding and the establishment of the symbiotic bacterial flora. However, in distinction to the respiratory diverticulum of the foregut, the allantois is shaped very early in development, prior even to formation of the embryonic endoderm and tailfolding. With the reorganization of the caudal area of the embryo at stage 10, a half of the allantois is drawn into the physique cavity. The early embryonic hindgut thus consists of a dorsal tubular area extending from the caudal intestinal portal to the cloacal membrane, and a ventral blindending allantois extend ing from the cloacal region into the connecting stalk. The barely dilated cavity, lined by endoderm, that cranially receives the enteric hindgut proper and the foundation of the allantoenteric diverticulum is termed the endodermal cloaca. It is closed ventrally by the cloacal membrane (endoderm against proctodeal ectoderm), and it additionally has, tran siently, a small recess of endoderm within the root of the tail, the postanal gut. As elsewhere, the hindgut, allantois and endodermal cloaca are encased in splanchnopleuric mesenchyme. The cloacal membrane is thus divided into anal (dorsal) and urogenital (ventral) membranes. The nodal centre of division is the positioning of the future perineal body, the functional centre of the perineum. Muscularis the muscularis is present and functioning by the eighth week, when peristaltic waves have been noticed. The specific orientation of the longitudinal muscle layer into taeniae coli occurs in the eleventh to twelfth weeks, when haustra seem. Serosa the development of the serosa of the gut is considered with the event of the peritoneal cavity (see below). Colon at start In the neonate, the colon is typically 66 cm lengthy and averages 1 cm in width. The caecum is relatively smaller than in the adult; it tapers into the vermiform appendix. The ascending colon is shorter in the neonate, reflecting the shorter lumbar region. The sigmoid colon may be so long as the transverse colon; it typically touches the inferior part of the anterior physique wall on the left and, in about half of neonates, part of the sigmoid colon lies in the right iliac fossa. The rectum is comparatively lengthy; its junction with the anal canal varieties at nearly a proper angle. The improvement of the massive intestine, whether derived from mid or hindgut, seems to be comparable. The proximal end of the colon could be first recognized at stage 15, when an enlargement of a neighborhood portion of intestine on the caudal limb of the midgut loop defines the creating caecum. The early endodermal lining of the colon seems stratified, and mitoses occur all through the layers. A sequence of longitudinal folds come up initially at the rectum and caecum, and later in the areas of colon between these two factors. The creating mucosa invagi nates into the underlying mesenchyme between the villi to type glands that increase in number by splitting longitudinally from the bottom upwards. With the absorption and disappearance of the anal membrane, the anorectum communi cates with the outside. The lower a part of the anal canal is formed from the proctodeal ectoderm and underlying mesenchyme, however its upper half is lined by endoderm. The twin origin of the anal canal is mirrored in its innervation: the endodermal portion is innervated by autonomic nerves, and the ectodermal proctodeum is innervated by spinal nerves.
Syndromes
Some patients additionally expertise an uncomfortable sensation of not with the flexibility to arteria fibularis buy 75 mg plavix visa management their physique temperature blood pressure chart template plavix 75 mg order online. It has been claimed that the vagi indirectly affect ventricular muscle through their effect on the atrioventricular node essential hypertension plavix 75 mg order with amex, the postganglionic parasympathetic innervation of the ventricles being sparse. The smaller branches of the coronary arteries are innervated mainly through the vagus, whereas the bigger arteries are mainly supplied by sympathetic fibres. Regional patterns of innervations could explain some particular types of cardiomyopathies similar to apical ballooning (Takotsubo cardiomyopathy). Pulmonary branches are motor to the circular easy muscle fibres of the bronchi and bronchioles, and are therefore bronchoconstrictor; synaptic relays happen within the ganglia of the pulmonary plexuses. The distribution of the vagi to the stomach viscera is described within the relevant chapters. Here, it provides off posterior bronchial branches that unite with rami from the second to fifth or sixth thoracic sympathetic ganglia to type the right posterior pulmonary plexus. Two or three branches descend from the inferior a half of this plexus on the posterior facet of the oesophagus to be part of a left vagal department and type the posterior oesophageal plexus. A vagal trunk containing fibres from both vagi leaves the plexus and runs inferiorly on the posterior floor of the oesophagus, coming into the abdomen by passing through the diaphragmatic oesophageal aperture. Left vagus the left vagus enters the thorax posterior to the left brachiocephalic vein, between the left common carotid (anterior) and the subclavian arteries (posterior). Posterior to the left hilum, it divides into the posterior bronchial branches, which unite with rami of the second to fourth thoracic sympathetic ganglia to form the left posterior pulmonary plexus. Two or three branches descend anteriorly on the oesophagus and be a part of with a ramus from the proper posterior pulmonary plexus to form the anterior oesophageal plexus. A trunk containing fibres from both vagi descends anterior to the oesophagus and enters the stomach Right vagus the right vagus nerve descends posterior to the inner jugular vein within the neck (p. It then descends via the superior mediastinum, at first posterior to the proper brachiocephalic vein, and then to the right of the trachea and posteromedial to the superior vena cava. The nerve next passes posterior to the proper major 982 Thymus via the oesophageal diaphragmatic aperture. Numerous branches from the anterior vagal and left sympathetic trunks are distributed to the descending thoracic aorta. This pathway transmits the everyday intense, excruciating ache of an intramural aortic haematoma from dissection or laceration. Superiorly, extensions into the neck are widespread, reflecting its bilateral embryonic origins from the third pharyngeal pouch (p. Its superior poles be part of at, and prolong above, the extent of the suprasternal notch; the left normally extends larger and is seen first behind the strap muscles during the preliminary phases of transcervical thymectomy. It generally reaches the inferior poles of the thyroid gland or even larger, and is related to the thyroid gland by the thyrothymic ligament. Inferiorly, the best lobe commonly lies between the right side of the ascending aorta and the best lung, anterior to the superior cava. Anteriorly, from superior to inferior, lie sternohyoid and sternothyroid, cervical fascia, the manubrium sterni, inside thoracic vessels and higher three costal cartilages. The pleurae lie laterally and the phrenic nerves are anterolateral and inferior; each buildings could additionally be injured throughout thymectomy. Posteriorly, the thymus is in touch with the vessels of the superior mediastinum (the left brachiocephalic vein and the inferior thyroid veins are normally partly embedded in the gland), the superior part of the thoracic trachea and the anterior cardiac surface (right atrium and ventricle). Thoracic surgeons performing thymectomy must pay attention to the anatomical variation in which the higher poles could lie posterior to the left brachiocephalic vein. Separated thymic tissue is commonly discovered scattered across the gland, and ectopic thymic rests are sometimes discovered in unusual mediastinal places. Small accessory nodules could happen in the neck, representing separated portions, detached throughout embryological descent, and generally reaching more superiorly than the thyroid cartilage. Capsular tissue might have adhesions to the fibrous pericardium, which is thinner superiorly and may both simply tear or require a restricted pericardotomy during thymectomy. Relations the thymus is largest within the early a half of life, significantly around puberty, and persists actively into old age regardless of considerable fibrofatty degeneration that generally hides the existence of persistent thymic tissue. The larger a half of the thymus lies in the superior and anterior mediastina; the inferior facet of the thymus reaches the level of the fourth costal cartilages. As no particular hilum exists, the arterial branches either travel along the interlobar septa earlier than getting into the thymus at the junction of the cortex and medulla, or they reach the thymic tissue immediately through the capsule. Trachea Cervical extensions of thymus Carotid arteries (low division) Veins Thymus, left lobe Thymus, proper lobe Right lung Thymic veins drain to the left brachiocephalic, internal thoracic and inferior thyroid veins, and sometimes instantly into the superior vena cava. One or more veins typically emerge medially from every lobe of the thymus to form a common trunk opening into the left brachiocephalic vein and require cautious ligation during thymectomy. Efferent lymphatics arise from the medulla and corticomedullary junction, drain through the extravascular areas, accompany the supplying arteries and veins, and finish in the brachiocephalic, tracheobronchial and parasternal nodes. Branches from the phrenic and descending cervical nerves (inferior roots of the ansa cervicalis) are distributed primarily to the capsule. The two lobes are innervated individually via their dorsal, lateral and medial features. During improvement and before its descent into the thorax, the thymus is innervated by the vagi in the neck. After its descent, the thymus receives a sympathetic innervation by way of fibres that journey alongside the vessels; postganglionic sympathetic terminations department radially and type a plexus with the vagal fibres at the corticomedullary junction. Many of the autonomic nerves are likely vasomotor, however different terminal branches (at least in rodents) ramify among the cells of the thymus, significantly the medulla, suggesting that they might produce other roles. The medulla contains a variety of several types of non-lymphoid cells, together with cells constructive for vasoactive intestinal polypeptide and acetylcholinesterase; massive non-myoid cells; and cells containing oxytocin, vasopressin and neurophysin, of attainable neural crest origin. These steps involve intimate interactions between thymocytes, primarily epithelial and antigen-presenting cells and chemical components in the thymic environment. The thymus can additionally be a part of the neuroimmunological and neuroendocrine axes of the physique, influenced by and influencing the merchandise of those axes. Its activity due to this fact varies throughout life under the influence of different physiological states, disease situations and chemical insults, corresponding to hormones, medication and pollutants. The thymus seems to be most lively between the ages of 3 and 6 months, when the highest variety of complete thymocytes are current (Weerkamp et al 2005). Originating prenatally, and growing in quantity throughout life, they maybe remove dying thymocytes as a outcome of their centres are eosinophilic and partly keratinized, and sometimes contain mobile particles. Myeloid lineage cells embrace monocytes at the corticomedullary junction, mature macrophages all through but notably within the cortex, and interdigitating dendritic (antigen-presenting) cells on the corticomedullary junction and within the medulla. Fibroblasts are discovered in the capsule, perivascular spaces and medulla but are rare in the cortex, except in the involute thymus. Myoid cells, that are relatively rare, are situated primarily in the medulla and on the corticomedullary junction. They are giant, rounded cells possessing a central nucleus surrounded by irregularly arranged bundles of myofilaments with unknown operate, although it has been instructed that their contractions might help the movement of lymphoid cells across or out of the thymus. General structure It is helpful to contemplate the embryological origins of the thymus in order to perceive its cellular group. It is derived from a selection of sources, together with epithelial derivatives of the pharyngeal pouches, mesenchyme, haemolymphoid cells and vascular tissue. Both thymic lobes have a free, fibrous connective tissue capsule, from which septa penetrate to the junction of the cortex and medulla, and partially separate the irregular lobules, that are each 0. The connective tissue septa kind a route of entry and exit for blood vessels and nerves, and carry efferent lymphatics. In each lobule, the cortex consists of a superficial subcapsular cortex (a narrow band of cells instantly beneath the capsule) and a more in depth primary cortex. The central medulla of both thymic lobes is continuous from one lobule to the next. They occupy the interstices of the epithelial reticulum, which they largely obscure in histological sections, and type 90% of the whole weight of the neonatal thymus. A distinct subcapsular zone homes the thymic stem cells and lymphoblasts undergoing mitotic division. The first stem cells to enter the thymus within the embryo come from the yolk sac and liver throughout their haemopoietic phases. The processes of thymocyte improvement and maturation to generate T cells depend upon the microenvironment offered by epithelial cells, dendritic cells, macrophages and fibroblasts. Over 95% of cortical thymocytes die inside the thymus; the surviving T cells migrate by way of the walls of venules and efferent lymphatics to enter the circulation and populate secondary lymphoid tissues (for additional particulars of thymocyte improvement, see p. Although differing in morphology, all of the epithelial cells of the thymus share a common origin from pharyngeal endoderm.
The definitive trabeculations blood pressure medication rebound effect plavix 75 mg generic amex, coarse in the proper ventricle however much finer within the left blood pressure 300 150 75 mg plavix generic overnight delivery, are first observed around the fortieth day of gestation; they seem initially in the partitions of each ventricles on the stage of the atrioventricular junction and develop in course of the apex of the heart blood pressure chart age 65 plavix 75 mg buy discount on-line. By the time the fetus is 10 weeks old, the trabeculations are a lot sparser, and are confined to the apical areas. This process of remodelling is achieved without the intervention of macrophages or inflammatory cells in the immediate interstitium. The ventricular myocardium, encompassing the trabeculations and exterior wall, possesses a chamber phenotype, the myocytes expressing, among different proteins, the fast-conducting gap-junctional proteins connexin forty (Cx40) and forty three, and atrial natriuretic peptide. This myocardium stops proliferating and differentiates into the fast-conducting peripheral ventricular conduction system, whereas the outer layer turns into extremely proliferative and types the compact layer of the ventricular wall, not expressing Cx40 and atrial natriuretic peptide, but still expressing Cx43. It displays a attribute bend, which has a proximal part arising from the growing proper ventricle, and a distal part that turns into continuous with the aortic sac beyond the pericardial reflections. Instead, it appears probable that cells are recruited from the second heart-forming area, and move by way of the outflow tract to contribute to the definitive proper ventricle. Subsequently, still extra cells are recruited from pharyngeal mesenchyme, passing proximal to the pericardial reflections and forming the intrapericardial elements of the arterial trunks. There remains much disagreement as to how best to describe these morphological components of the outflow tract. Some authors have labelled the proximal myocardial part the conus, calling the distal part the truncus, and the intrapericardial portion of the outflow tract the aortic sac. The left ventricle develops from the stem of the Y-shaped heart; the best ventricle develops later, downstream relative to the left ventricle, when more myocardium has been added to the cardiac tube. As a results of the looping of the guts tube, the best ventricle is positioned on the proper of the left ventricle, which is a prerequisite for the suitable reference to the increasing atrial component of the center. Because the terms conus and truncus have been inconsistently used in literature, we choose simply to describe proximal and distal components of the myocardial outflow tract, and to describe, when it appears, an intrapericardial arterial portion of the outflow tract, this part interposing between the muscular element and the ventral aorta, the distal junction occurring on the pericardial reflections. The latest finding that the stem of the heart tube contains precursor cells solely for the left ventricle makes it essential to adopt descriptions that follow dynamic events, somewhat than persevering with to use static names. Cells that, initially, are discovered within the ventricular outflow tract subsequently become cells of the right ventricle. Furthermore, working myocytes can simply be distinguished from the primary myocytes of the straight coronary heart tube. The primary myocardium is smoothwalled, whereas the developing myocardium of the ventricles is trabeculated, and expresses specific markers corresponding to atrial natriuretic peptide and Cx40 and Cx43. Moreover, within the inner curvature of the ventricular loop, the walls of the outflow tract and atrioventricular canal fade into each other without a clear boundary. It is inside this ventricular a half of the primary coronary heart tube that the cushions of the atrioventricular canal and the outflow tract must obtain acceptable connections with the muscular ventricular septum in order to divide this a part of the tube into left and proper compartments. It is, none the much less, the remodelling of this inside curvature that sets the scene for the completion of cardiac septation. All areas of the early embryonic heart tube possess poorly coupled cells and show intrinsic automaticity, thus permitting slow propagation of the depolarizing impulses alongside the cardiac tube, and producing matching peristaltic waves of contraction that push the blood in an antegrade path. This tissue has been called major myocardium, distinguishing it from the quickly conducting and well-developed working myocardium of the atrial and ventricular chambers. An grownup kind of electrocardiogram may be recorded from such hearts, displaying rapid atrial depolarization, a period of atrioventricular delay, and speedy ventricular depolarization. The electrocardiographic tracings reflect the event of fast-conducting components within a slowly conducting coronary heart tube, i. The newly developed working myocardium expresses atrial natriuretic factor, together with the hole junctional proteins Cx40 and Cx43, which permit fast conduction. The slowly conducting atrioventricular canal, interposed between the atrium and the ventricle, and the outflow tract positioned between the ventricle and the good arteries, are the components that include the endocardial cushions. These are in a position to function as sphincteric valves, because of their prolonged duration of contraction. These parts retain their operate till the definitive leaflets of the one-way valves have been sculpted from the cushions. The major myocardium of the atrioventricular canal is finally incorporated into the atrial vestibules at the same time as the formation of the atrioventricular valves, becoming sequestrated on the atrial side of the atrioventricular junctions between 6 and 12 weeks of growth. The combined motion of the transcription factors Tbx5 and Nkx2�5 is required for the formation of the myocardium of the atrial and ventricular chambers. Tbx5 is expressed in a gradient over the guts tube, lowering in focus from caudal to cranial, and may impose positional information. Localized expression of the transcriptional repressors Tbx2 and Tbx3 within the influx tract, the floor of the atrium, the atrioventricular canal, the internal curvature of the ventricular area, and the outflow tract prevents the differentiation of primary into working myocardium. Tbx2 and Tbx3 effectively compete for binding to the promoters of the chamberspecific genes, corresponding to atrial natriuretic factor, Cx40 and Cx43. The remaining main myocardium of these regions initially induces the endocardium to undergo epithelial to mesenchymal transition, by which course of the cardiac cushions turn into filled with mesenchyme. The myocardium additionally participates within the alignment of the atrial and ventricular chambers (which is essential for correct cardiac septation, and is guided by the fusing cardiac cushions); it varieties the conduction system, together with the sinus and atrioventricular nodes, the atrioventricular bundle, the ground of the developing right atrium (the internodal region), and the whole thing of the atrioventricular canal. In the early chamber-forming heart of the mouse, Tbx3 is expressed in the atrioventricular canal, the ground of the atrium and around the orifices of the systemic venous tributaries, however not in the dorsal mesocardium surrounding the entrance of the pulmonary vein. During subsequent improvement, the area of expression of Tbx3 expands from the atrioventricular canal to kind a crescent on the crest of the ventricular septum. The dorsal aspect of this crescent develops into the atrioventricular bundle, while the atrioventricular node is shaped on the dorsal junction with the atrioventricular canal. Indeed, the event of the conduction system of the guts is inextricably associated with the event of the fundamental building plan for the heart. The conduction system is best defined because the system that initiates and conducts the sinus impulse. In mammals, it encompasses the sinuatrial node, the atrioventricular node, the atrioventricular bundle, the bundle branches and their terminal ramifications. The nodes and the atrioventricular bundle can be considered the central conduction system, whereas the bundle branches and their ramifications characterize the peripheral ventricular conduction system. After an essential period of atrioventricular delay, the impulse travels rapidly through the atrioventricular conduction axis and the peripheral ramifications to attain the ventricular myocardium, which is then rapidly depolarized. Following repolarization, the sequence recurs in infinite fashion all through the life of the person. In order to produce highly effective synchronous contractions, the working myocardium of the chambers must also, of necessity, conduct quickly, whereas to act as a pacemaker, the cells of the nodes must be poorly coupled, and therefore show slow conduction. The vertebrate heart is myogenic, implying that every one cardiomyocytes have the capacity to generate and conduct the depolarizing impulse. Because cardiac myocytes are electrically coupled, the cells with the very best pacemaking activity take the lead. In the shaped regular heart, the main pacemaker is at all times inside the sinus node. A, At stage thirteen with the truncus arteriosus reflected to the proper, the interventricular ring marks the area of the primary heart tube. B, the truncus arteriosus, now divided into the pulmonary trunk and aorta, is presented between the proper and left atria, which increase lateral to it. The proper atrium is now positioned totally above the proper ventricle, and the outflow tract has expanded to the left; the left ventricle has access to the aorta. C, the position of the unique main heart tube ring indicated within the formed heart. Even so, regular growth of the center requires that each one cardiac compartments obtain an enough amount of blood. To this finish, even earlier than start, the systemic blood of the right atrium is guided to the left atrium in order that the left half of the guts and the mind is supplied with a traditional circulate of blood. The walls that separate the best and left sides of the heart are largely shaped in the fourth and fifth weeks of development. Some time later, not solely the parts of the primary heart tube � particularly, the atrioventricular canal and the outflow tract � but additionally the atrial and ventricular chambers, must be separated physically into proper and left halves. The concept accounts significantly properly for the morphology and disposition of the atrioventricular node and bundle in hearts with straddling tricuspid valves, with double inlet left ventricles, and with congenitally corrected transposition. Internal separation into proper and left atria is mainly effected by development of two septa, coupled with remodelling of the venous compartments. The forefront of the septum primum is roofed by a mesenchymal cap in continuity dorsally with extracardiac mesenchyme (mediastinal mesenchyme) derived from the dorsal mesocardium which types the vestibular backbone, or spina vestibule, also called the dorsal mesenchymal protrusion. The ventral horn of the septum primum reaches the ventral (cranial) atrioventricular cushion, while the dorsal horn reaches the dorsal (caudal) cushion. Thus the primary atrial foramen, the foramen or ostium primum, is entirely surrounded by mesenchyme derived from endocardium. As the foramen primum diminishes in size, the upper margin of the septum primum perforates by apoptosis and, thus, proper to left shunting of blood continues via a secondary foramen, the foramen or ostium secundum.

The terminal part of the thoracic duct emerges from the posterior aspect of the aorta and oesophagus blood pressure 160 over 100 plavix 75 mg cheap on line, ascending between the left subclavian and carotid arteries prehypertension at 30 plavix 75 mg effective. The superior (extrapericardial) half of the superior vena cava and its major tributaries are situated on a extra superficial airplane posterior to the manubrium and the origins of sternothyroid inferiorly hypertensive retinopathy cheap 75 mg plavix with visa, and sternohyoid superiorly. An enlarged thyroid gland may prolong inferiorly between the sternum and the brachiocephalic veins; its surgical excision requires due diligence from attainable venous adherence. The origins of longus colli (inferior indirect and vertical intermediate portions) are the deepest parts of the superior mediastinum. Strictly talking, the mediastinum is the visceral compartment between the two lungs and consists of the mediastinal pleura. It communicates with the neck through the superior thoracic aperture and with the extraperitoneal, extrapleural and epidural spaces. Beyond every pulmonary hilum, the mediastinum merges into the lung interstitium, incorporating the bronchial tree with its accompanying neurovascular bundles and the pulmonary vasculature. The posterior mediastinal boundary is longer on account of the oblique disposition of the superior thoracic aperture and the diaphragmatic curvature posteroinferiorly. Detailed accounts of mediastinal contents are included with descriptions of the respiratory organs (Ch. The reflection of the costomediastinal pleurae follows a line that passes from the sternoclavicular joints in an inferomedial direction, to join the midline on the posterior facet of the sternal angle. It narrows above the fourth costal cartilages where the pleural sacs converge, and accommodates loose connective tissue, the sternopericardial ligaments, a couple of lymph nodes, the mediastinal branches of the interior thoracic artery, and generally part of the thymus gland or its degenerated remains. The pericardium and the heart are routinely approached by both a complete median or partial sternotomy. The sternopericardial ligaments and the pleural reflections are simply separated by blunt dissection. In case of pericardial tamponade, the pericardial cavity may be easily drained by way of a subxyphoid method, both surgically or via needle pericardiocentesis. The brief thoracic part of the inferior vena cava, each extra- and intrapericardial segments, extends between the vena caval aperture of the diaphragm and its termination in the best atrium. The mediastinal pleura is steady with the visceral pleura on the degree of the hilum, which is where the lateral boundary of the center mediastinum is conventionally situated. The fibrous pericardium lies on, and is fused with, the anterior two-thirds of the central tendon of the diaphragm. Subdivisions of the mediastinum tracheal bifurcation, pericardium and pulmonary vessels, and posteriorly by the our bodies of the fifth to the twelfth thoracic vertebrae. The arched posterior third of the central portion of the diaphragm constitutes the anteroinferior limit of the posterior mediastinum laterally as the mediastinal pleurae come close together. Two pleural recesses, the interaortico-oesophageal and interazygo-oesophageal recesses, intercalate from the left and proper sides between the aorta and oesophagus and the azygos vein and oesophagus, respectively. The posterior mediastinum contains the descending thoracic aorta (on the left facet of the spine), the oesophagus (median, but positioned anterior to the aorta inferiorly) and, more posteriorly, the azygos and hemiazygos venous methods, the thoracic duct, lymph nodes, right and left sympathetic chains and thoracic splanchnic nerves. The vagal trunks course adjoining to the oesophagus; the anterior trunk is constituted primarily from the left vagus nerve and the posterior primarily from the right vagus nerve. There are numerous communications between the posterior mediastinum and the abdomen. These are: the oesophageal aperture (also transmits the vagal trunks) on the stage of the tenth thoracic vertebra; the aortic aperture (also transmits the thoracic duct and sometimes the azygos vein) on the level of the twelfth thoracic vertebra; apertures inside the diaphragmatic crura that transmit the thoracic splanchnic nerves; apertures deep to the medial lumbosacral arches for the sympathetic chains; and minute openings within the central tendon of the diaphragm that transmit small veins. All openings symbolize potential communication sites for suppurative or neoplastic processes. The former is more more likely to be infected than any of the opposite potential tissue spaces within the head and neck, communicating with the retropharyngeal and pretracheal spaces, so reaching the superior mediastinum after which the anterior a part of the inferior mediastinum (see Chs 29 and 31). The airplane between the buccopharyngeal and prevertebral fasciae is a highway for unfold of air and gastric contents between the neck and mediastinum after oesophageal harm (Wind and Valentine 2013). The carotid sheath, containing the carotid arteries, jugular veins and vagus nerves, represents another potential route of communication. Great vessels of the superior mediastinum the aortic arch, descending thoracic aorta, pulmonary trunk and superior vena cava are described in Chapter 57. When present, the azygos lumbar vein ascends anterior to the higher lumbar vertebral bodies and passes either posterior to or by way of the proper diaphragmatic crus or traverses the aortic hiatus to the right of the cisterna chyli. In the absence of a lumbar azygos vein, this widespread trunk may continue as the azygos vein proper. The azygos vein passes to the best, posterior to the right crus of the diaphragm, and ascends in the posterior mediastinum to the extent of the fourth thoracic vertebra, the place it arches anteriorly, superior to the right pulmonary hilum, and joins the posterior facet of the superior vena cava, just superior to its pericardial incorporation. In its course, the azygos vein lies anterior to the our bodies of the decrease eight thoracic vertebrae, anterior longitudinal ligament and proper posterior intercostal arteries. Right lateral relations are the right sympathetic chain, the proper larger splanchnic nerve, lung and pleura. Left lateral relations are the thoracic duct, aorta and, the place the vein arches anteriorly, the oesophagus, trachea and right vagus. The recess is dextroconvex under the age of 6 years, non-concave (equally divided between straight and convex) between 6 and 12 years and concave, as in adults, after the age of 12 years (Miller et al 1993). Its main tributaries are the proper intercostal veins (the first drains into the best brachiocephalic vein and the second, third and fourth kind a typical trunk, the superior intercostal vein), the right ascending lumbar and subcostal veins, mediastinal, oesophageal, pericardial and right bronchial veins, and the hemiazygos and accessory hemiazygos veins. Numerous anastomoses exist between the tributaries and the primary trunks of the azygos, hemiazygos and accessory hemiazygos veins, the inferior vena cava and the vertebral venous plexuses. On the proper facet, that is the upper margin of the right upper lobe bronchus; the majority of nodes in this area tend to be positioned anterolateral to the trachea. On the left aspect, the nodes are situated beneath the upper margin of the aortic arch and above the margin of the left upper lobe bronchus. It originates in an analogous fashion (from the union of the left lumbar ascending and subcostal veins) but reveals extra variability; it might also join with the left renal vein via the equivalent of the lumbar azygos vein. It receives the decrease three left posterior intercostal, mediastinal and oesophageal veins. Oesophagus, cervical half Thyroid gland, proper lobe Common carotid artery Brachiocephalic trunk Subclavian artery Superior vena cava Trachea Superior tracheobronchial nodes Azygos vein Accessory hemiazygos vein the accessory hemiazygos vein functions as the left-sided mirror image of the superior portion of the azygos vein. It drains the fifth to eighth posterior intercostal veins and sometimes the left bronchial veins, and often terminates within the azygos vein after crossing the seventh thoracic vertebra. The first posterior intercostal vein drains instantly into the left brachiocephalic vein, whereas the second to the fourth drain not directly to the accessory hemiazygos vein through the left superior intercostal vein. The origin, course, tributaries, anastomoses and termination of the azygos system of veins are all extremely variable. The left channel may be absent or underdeveloped, permitting direct drainage of the left intercostal veins into the azygos and/or the termination of the accessory hemiazygos into the left brachiocephalic vein. Left inferior pulmonary vein Posterior mediastinal nodes Oesophagus, thoracic half 7 Superior tracheobronchial nodes Right pulmonary artery Right inferior pulmonary vein Posterior mediastinal nodes Pulmonary arteries and veins the pulmonary vessels are described on pages 959 and 960. Inferior vena cava Mediastinal lymph nodes For the needs of staging lung most cancers, thoracic surgeons classify the mediastinal lymph nodes into regional lymph node stations, which are outlined as shown in Table 56. Pulmonary nodes turn out to be continuous with the bronchopulmonary nodes, and these, in turn, merge with the inferior and superior tracheobronchial nodes, which are steady with the paratracheal group. The tracheobronchial nodes drain the lungs, bronchi, the thoracic a half of the trachea, and coronary heart, and also receive efferents from the posterior mediastinal nodes. Mediastinum In congenital interruption of the inferior vena cava or acquired thrombosis, the azygos system provides an alternative pathway for venous drainage. Metastatic involvement of those lymph nodes has necessary prognostic implications and influences the choice of therapy (Mountain and Dresler 1997). The staging system for lung most cancers classifies involvement of ipsilateral hilar lymph nodes as N1, ipsilateral mediastinal lymph nodes as N2, contralateral mediastinal or hilar nodes as N3 and supraclavicular/scalene nodes as M1 (distant metastases). It often originates anterior to the primary or second lumbar vertebrae, where the intestinal and two lumbar lymph trunks be a part of to form the cisterna chyli. It continues upwards, first posterior to the aortic arch adjacent to the left aspect of the oesophagus, then posterior to the left subclavian artery in the superior mediastinum. In the space between longus colli, the anterior scalene muscular tissues and the pleural dome, the duct usually arches three or four cm superior to the clavicle, crossing anterior to the vertebral vessels, the left sympathetic trunk, the vertebral ganglion, the thyrocervical trunk and the left phrenic nerve. In some patients, two thoracic ducts exist within the mediastinum, and occasionally a single thoracic duct may empty into rightsided venous constructions, the latter disposition being extra frequent in individuals with an aberrant proper subclavian artery (the latter originating from the distal aortic arch ascending posterior to the oesophagus). When present as a single channel, the thoracic duct is 5 mm in diameter at its origin, narrows to 2�3 mm at mid-thoracic level and then widens once more at its termination. Alternatively, it might divide into two or three branches that finally reunite or drain into both the left and proper venous methods. The duct seems sinuous and has valves throughout its length; a bicuspid valve at its termination might stop the backflow of blood. As it passes by way of the mediastinum, the thoracic duct also receives non-chylous lymph from tributaries that drain areas of the pulmonary parenchyma and parietal pleura.

The diaphragm is relatively flat centrally and domed peripherally blood pressure tool best plavix 75 mg, rising larger on the proper facet than on the left heart attack vs panic attack purchase plavix 75 mg without prescription, an asym metry that displays the relative densities of the underlying liver and gastric fundus blood pressure medication ringing in ears plavix 75 mg purchase without prescription, respectively. From its most superior point on both sides, the diaphragm slopes inferiorly to its costovertebral attachments; this slope is most marked posteriorly, where the space between the dia phragm and the posterior wall of the thorax is very narrow. During quiet respiration in the erect position, diaphragmatic tour is about 2 cm in both sexes, increas ing to around 7 cm throughout deep breathing (Boussuges et al 2009); values are larger in men and possibly enhance additional in the supine position (Takazakura et al 2004). Inferiormediastinum the inferior mediastinum is divided into three elements: anterior, in front of the pericardium; center, containing the pericardium and its contents (Ch. AnteriormediastinumThe anterior mediastinum exists solely on the left side the place the left pleura diverges from the midsternal line. It is bounded anteriorly by the sternum, laterally by the pleurae, and poste riorly by the pericardium. Its anterior wall is fashioned by the left transversus thoracis and the fifth to seventh left costal cartilages. It incorporates a amount of unfastened areolar tissue, lymphatic vessels that ascend from the convex floor of the liver, two or three anterior mediastinal lymph nodes, and the small media stinal branches of the interior thoracic artery. Other constructions that cross between the thorax and stomach include the right and left vagi, phrenic and subcostal nerves, thoracic duct, sympathetic trunks, thoracic splanchnic nerves, right and left superior epigastric arteries, and the hemiazygos and accent hemiazygos veins. MiddlemediastinumThe middle mediastinum is the broadest a part of the interpleural house; it contains the center enclosed in the pericar dium; the ascending aorta; the decrease half of the superior vena cava with the azygos vein opening into it; the bifurcation of the trachea and the best and left principal bronchi; the pulmonary artery dividing into its two branches; the best and left pulmonary veins and phrenic nerves; and a few bronchial lymph nodes. Posteriormediastinum the posterior mediastinum is an irregular triangular space, bounded anteriorly by the pericardium above and the posterior surface of the diaphragm below, posteriorly by the vertebral column from the lower border of the fourth to the twelfth thoracic vertebrae, and laterally by the mediastinal pleura. It contains the tho racic part of the descending aorta, the azygos and hemiazygos veins, the vagus and splanchnic nerves, oesophagus, thoracic duct and lymph nodes. Each encloses a lung and its associated bron chial tree, and vessels, nerves and lymphatics (Ch. The outer layer of the sac, the parietal pleura, strains the corresponding half of the thoracic wall and covers a lot of the diaphragm and structures occupying the middle region of the thorax. The inside or visceral layer is more delicate and adheres intently to the pulmonary floor, follow ing the interlobar fissures. The two layers are continuous with one another around the hilar buildings, and stay in shut, although sliding, contact at all phases of respiration. The potential space between them is the pleural cavity, which is maintained at a adverse strain by the inward elastic recoil of the lung and the outward pull of the chest wall. Additional contributions come from vessels that offer the proximal muscle tissue of the upper limb, namely: suprascapular, superficial cervical, thoracoacromial, lateral thoracic and subscapular arteries. The detailed arterial provide of the thoracic viscera is described with the viscera. The small anterior intercostal veins are tributaries of the internal thoracic and musculophrenic veins; the inter nal thoracic veins drain into the appropriate brachiocephalic vein. The posterior intercostal veins drain backwards, and most drain immediately or indirectly into the azygos vein on the right and the hemiazygos or hemiazygos veins on the left. The azygos veins exhibit nice variation of their origin, course, tributaries, anastomoses and termination. Intercostal nerves are dis tributed primarily to the thoracic and belly walls. The greater a part of the first thoracic ventral ramus passes into the brachial plexus, together with a variable proportion of the second. The subsequent 4 ventral provide only the thoracic wall, and the lower five provide both thoracic and belly walls. Communicating branches hyperlink the inter costal nerves posteriorly in the intercostal areas, and the lower five nerves communicate freely in the stomach wall. The supraclavicular branches of C4 from the cervical plexus internal vate the pores and skin over the clavicle and may talk with the anterior cutaneous branches of the second thoracic ventral ramus (p. Lymph vessels from deeper tissues of the thoracic partitions drain primarily to the parasternal, intercostal and diaphragmatic lymphatic nodes. The upper eleven lie between the ribs (intercostal nerves), and the twelfth lies beneath the last rib (subcostal nerve). Preganglionic sympathetic axons originate from neurones within the lateral gray column of the spinal cord from T1 to L2, and leave the spinal twine with the corresponding ventral roots as white rami communicantes. Some enter the sympathetic trunk, the place they either synapse in their segmental ganglion, or ascend or descend in the trunk to synapse in cervical or lumbar ganglia. Axons destined for the cervical ganglia are derived from preganglionic neurones in T1. In adult males, the nipple is often sited both within the fourth intercostal area or over the fifth rib in the midclavicular line, roughly 20 cm from the sternal notch and midclavicular level (Beckenstein et al 1996). Vagusnervesinthethorax Preganglionic parasympathetic fibres come up from neuronal cell bodies within the dorsal motor nucleus of the vagus in the medulla. Those destined for the thoracic viscera journey in the pulmonary, cardiac and oesopha geal branches of the vagus and synapse in minute ganglia within the visceral walls. Axons travelling in cardiac branches be a part of the cardiac plexuses and synapse in ganglia distributed over each atria; when stimulated, they gradual the cardiac cycle (Ch. The sternum could additionally be felt all through its size within the midline, although laterally it could be lined by pectoralis major. The jugular (supraster nal) notch is palpable within the midline on the superior sternal border and usually lies on the level of the junction between the second and third thoracic vertebrae. The cartilaginous rings of the trachea are palpable immediately superior to the notch, utilizing a posteriorly directed finger. The manubriosternal angle is more pronounced within the male than within the female, and is palpable on the junction of the manubrium with the sternal body. It serves as a useful landmark as a outcome of it signifies the level of the sternal airplane and the medial ends of the second costal cartilages, and so offers an correct level at which to start counting ribs. In the overwhelming majority of adults, the sternal angle is positioned between the fourth tho racic vertebra and the upper half of the fifth thoracic vertebra, with a spread from the lower half of the second thoracic vertebra to the decrease half of the sixth thoracic vertebra, a linear distance of about eight cm; the aircraft lies at a barely larger vertebral level in girls. The xiphisternal joint and xiphoid process are palpable at the inferior end of the sternum; the joint often lies on the level of the ninth thoracic vertebra. Posteriorly, the free ends of the eleventh and twelfth ribs may be Autonomicplexusesinthethorax Cardiac plexus the cardiac plexus has a superficial component inferior to the aortic arch, mendacity between it and the pulmonary trunk, and a deep half between the aortic arch and tracheal bifurcation (Ch. The superficial half is shaped by the cardiac department of the left superior cervical sympathetic ganglion and the lower of the two cervical cardiac branches of the left vagus. The deep part is fashioned by the cardiac branches of the cervical and higher thoracic sympathetic ganglia and of the vagus and recurrent laryngeal nerves. Branches from the cardiac plexuses also form the left and proper coronary and atrial plexuses. Pulmonaryplexus the pulmonary plexuses are anterior and poste rior to the opposite constructions on the hila of the lungs (Ch. They are formed by cardiac branches from the second to fifth (or sixth) thoracic sympathetic ganglia and from the vagus and cervical sympathetic cardiac nerves. Vagal fibres both pass by way of the plexus or are given off immediately by the vagus in the thorax. All fibres relay within the oesophageal wall and are motor to the smooth muscle within the decrease oesophagus and secretomotor to mucous glands within the oesophageal mucosa. Vasomotor sympathetic fibres arise from the higher six thoracic spinal cord segments. Those from the higher segments synapse in cervical ganglia; postganglionic axons innervate the vessels of the cervical and higher thoracic oesophagus. Fibres from the lower segments pass on to the oesophageal plexus or to the coeliac ganglion, the place they synapse; postganglionic axons innervate the vessels of the distal oesophagus. The accuracy of some older descrip tions of clinically important floor landmarks, based mostly on cadaveric or radiographic studies, has been questioned just lately (Hale et al 2010). The tail of the breast extends in the path of the axilla along the infero lateral border of pectoralis main (Ch. Key: 1, right acromioclavicular joint; 2, clavicle and mid-clavicular line (dashed black); three, apex of proper lung, positioned posterior to the medial third of the clavicle; four, sternal notch of manubrium sterni: the trachea could additionally be situated right here by posterior palpation; 5, sternoclavicular joint: marks the junction of the interior jugular and subclavian veins to kind the brachiocephalic vein; 6, zone of formation of the superior vena cava: from first intercostal house to second costal cartilage level (78% of subjects, white zone); 7, sternal angle: marks the extent of the sternal airplane and the second costal cartilage; 8, pectoralis major and the anterior axillary fold; 9, horizontal fissure; 10, right oblique fissure; eleven, decrease anterior border of the right lung: typically, both the sixth intercostal space or the seventh rib within the mid-clavicular line; 12, decrease anterior border of the left lung: typically, both on the fifth rib or fifth intercostal house in the mid-clavicular line; thirteen, xiphisternum; 14, costal margin; 15, tenth costal cartilage, forming the lower a half of the costal margin. The levels of the spinous processes of the third, ninth and twelfth thoracic vertebrae and the first lumbar vertebra are indicated within the midline. Key: 1, border of the left lung; 2, indirect fissure: passes anteroinferiorly from the spinous strategy of the third thoracic vertebra to cross the fifth rib in the midaxillary line. The upper lobe sits superiorly and the decrease lobe inferiorly; 3, decrease border of the lung: that is typically located at stage of the twelfth thoracic vertebra but could additionally be lower, at the degree of the primary lumbar vertebra, adjacent to the vertebral column at end tidal inspiration. Dashed blue traces indicate the range of levels for the decrease border of the lung (ninth thoracic vertebra to first lumbar vertebra); 4, twelfth rib: could be traced superomedially to assist identification of the spinous process of the twelfth thoracic vertebra. Posteriorly, the spinous processes of the thoracic vertebrae are palpable; the spinous means of the primary thoracic vertebra sits below that of the seventh cervical vertebra (vertebra prominens) and is often extra outstanding.
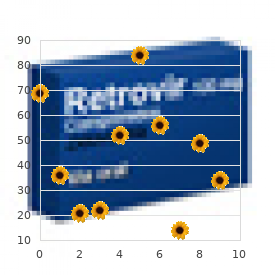
Different authors have used the identical eponym for various fasciae; different eponyms have been used to check with hypertension lifestyle modifications buy plavix 75 mg without a prescription the same fascia heart attack 6 hours plavix 75 mg generic with visa. It is an avascular layer that permits a dissection airplane to be developed arteria pudenda externa cheap 75 mg plavix with visa, and likewise limits the spread of disease. The retropancreaticoduodenal fascia and the retrocolic/retromesocolic fascia (right and left) are fusion fascias, and delimit their respective compartments. They were first described intimately by the Austrian anatomist Carl Toldt, and solely later reported within the English literature (Congdon et al 1942). Traditional compartmental anatomy of the retroperitoneum divides it into the anterior and posterior pararenal areas, and the perirenal area. This is an oversimplification and is unable to clarify all patterns of disease containment or spread. The smallest set of compartments adequate to clarify most such phenomena is as follows. The pericolic spaces contain a variable amount of fats and are limited anteriorly, superiorly and laterally by the colonic serosa. Inferiorly, the pericolic areas are steady with the retroperitoneal areas of the iliac fossae. Posteriorly, each pericolic space is proscribed by a fusion fascia formed by the right leaf of the embryonic mesocolon fusing to the left leaf of the embryonic duodenal mesentery and embryonic retroperitoneum further laterally. This retrocolic fascia (of Toldt) (Culligan et al 2013, Culligan et al 2014) varieties the classic bloodless airplane of dissection when performing a hemicolectomy. Its airplane is entered by incising the junction of the colonic serosa with the parietal peritoneum at the white line (of Toldt) within the paracolic gutter. Radiologically, the retrocolic fascia may be indistinguishable from the anterior perirenal fascia when lateral to the duodenum and pancreas. Variation in colonic retroperitonealization might produce a free mesocolic pedicle as an alternative (most commonly seen on the caecum). Perirenal space the paired perirenal space is bounded by the perirenal fascia, which envelops the kidney and suprarenal gland on each side. The perirenal fascia can normally be identified on cross-sectional imaging as a skinny layer surrounding the kidney and suprarenal gland, separated from the renal capsule by a variable quantity of perirenal fat. Inferiorly, the perirenal house continues down around the ureter however becomes progressively narrower and may or may not prolong into the pelvic retroperitoneum. Medially, the 2 perirenal areas could interconnect anterior to the aorta and inferior vena cava (Kneeland et al 1987). The existence of a fascial partition separating the kidney and ipsilateral suprarenal gland throughout the perirenal fascial envelope is controversial (Amin et al 1976). Lateroconal fascia Lateroconal fascia was initially defined because the fascial layer extending from the junction of the anterior and posterior perirenal fasciae to the parietal peritoneum in the lateral paracolic gutter (Congdon and Edson 1941). The particular person bones are the decrease two ribs, the twelfth thoracic and five lumbar vertebrae, and the sacrum and ilium, along with their interconnecting ligaments (Chs 43, 53). The potential compartment between the posterior layer of perirenal fascia and the thoracolumbar and psoas fasciae on all sides is the posterior pararenal house. When the ascending or descending colon is retrorenal (an anatomical variant), the colon and pericolic house lie in a groove between the posterior layer of perirenal fascia and the posterior pararenal area. Quadratus lumborum Quadratus lumborum is an irregularly shaped quadrilateral muscle, broader at its inferior attachment than superiorly. Attachments the inferior attachment is by aponeurotic fibres to the iliac crest over an space 5�7 cm lateral to the tip of the L4 transverse course of and/or the iliolumbar ligament. The superior attachment is to the lower anterior surface of the twelfth rib, the lateral surface of the twelfth thoracic vertebra, and the apices of the transverse processes of the higher 4 lumbar vertebrae. Fascicles differ in number and measurement however are organized in three layers: anterior, middle and posterior (Phillips et al 2008). Peripancreatic space the peripancreatic house contains the duodenum and pancreas along with the origins of the superior mesenteric vessels and the retroperitoneal segments of the widespread bile duct, portal vein and hepatic artery. The posterior boundary is a fusion fascia shaped by fusion of the embryonic duodenal mesentery to the embryonic retroperitoneum (Dodds et al 1986). The fascia varieties a comparatively cold dissection plane, used to mobilize the duodenum and head of the pancreas. At the tail of the pancreas, the peripancreatic space lies in continuity with the splenorenal ligament. Vascular provide Quadratus lumborum is equipped by branches of the lumbar arteries, the arteria lumbales imae from the median sacral artery, the lumbar department of the iliolumbar artery, and branches of the subcostal artery. Innervation the muscle is innervated by the ventral rami of the twelfth thoracic and upper three or four lumbar spinal nerves. Pericolic areas the ascending and descending pericolic spaces are slim compartments surrounding the respective components of the colon and in continuity Actions Quadratus lumborum fixes the twelfth rib, and acts as a muscle of inspiration by serving to to stabilize the lower attachments of the diaphragm. With the pelvis fastened, unilateral contraction flexes the vertebral column to the identical side, and bilateral contraction in all probability helps to prolong the lumbar part of the vertebral column. These actions on the lumbar backbone are reported to be weak (Phillips et al 2008) and but the muscle undergoes considerable hypertrophy in some sporting activities (Ranson et al 2008). The subcostal, iliohypogastric and ilioinguinal nerves lie on the fascia anterior to the muscle, certain all the means down to it by the medial continuation of the transversalis fascia. The fusion fasciae forming the boundaries of the peripancreatic space are thickened via continual irritation and are easily seen. Key: 1, neck of pancreas; 2, gasoline in anterior a part of assortment (outlining peripancreatic space); 3, fluid and debris in posterior (dependent) a half of assortment (outlining peripancreatic space); 4, retropancreatic fusion fascia (anterior perirenal fascia fused to right leaf of mesoduodenum); 5, anterior peripancreatic fascia fused to proper leaf of left mesocolon; 6, anterior peripancreatic fascia deep to left mesocolon and collapsed lesser sac; 7, anterior peripancreatic fascia fused to peritoneum of lesser sac in gastric bed; eight, superior mesenteric artery; 9, stomach aorta; 10, inferior vena cava; 11, left renal vein; 12, left kidney parenchyma; 13, left perirenal area (not distinguishable from left posterior pararenal space); 14, right kidney parenchyma; 15, right perirenal space (not distinguishable from right posterior pararenal space); 16, upper L2 vertebral body; 17, splenic flexure; 18, stomach (elevated and compressed by collection); 19, gallbladder; 20, right lobe of liver (segments 5 and 6); 21, right crus of diaphragm; 22, origin of left psoas main; 23, left quadratus lumborum; 24, left erector spinae group. Key: 1, inferior part of body and uncinate process of pancreas; 2, distal second a part of duodenum; three, third a part of duodenum; 4, peripancreatic area collection (around and anterior to pancreas and duodenum); 5, superior mesenteric vein; 6, superior mesenteric artery; 7, small bowel mesentery; 8, a half of assortment dissecting into transverse mesocolon; 9, transverse mesocolon (fused to larger omentum); 10, transverse colon; 11, assortment dissecting behind ascending colon; 12, ascending colon; 13, collection (with gas) dissecting behind descending colon; 14, descending colon; 15, left kidney parenchyma; 16, left perirenal space; 17, left posterior perirenal fascia (normal thickness, due to this fact faint); 18, left posterior pararenal house; 19, right kidney parenchyma; 20, right perirenal house; 21, right posterior perirenal fascia; 22, right posterior pararenal area; 23, anterior pararenal fascia (thickened by way of chronic inflammation); 24, upper L4 vertebral body; 25, stomach aorta; 26, inferior vena cava; 27, right psoas major; 28, left quadratus lumborum; 29, left erector spinae group. Key: 1, neck of pancreas; 2, gas in anterior a half of collection; three, fluid in posterior a part of assortment; four, coeliac trunk; 5, superior mesenteric artery; 6, left renal vein; 7, abdominal aorta; 8, diaphragmatic crura; 9, left lobe of liver; 10, antrum of stomach (collapsed); eleven, a half of assortment dissecting into transverse mesocolon; 12, transverse colon; 13, part of collection dissecting into small bowel mesentery; 14, third part of duodenum. Key: 1, physique of pancreas; 2, fluid assortment; 3, fundus of abdomen (containing oral contrast); 4, body of abdomen (containing oral contrast and displaced); 5, left anterior perirenal fascia fused with retropancreatic fascia; 6, left anterior perirenal fascia fused with right leaf of left mesocolon (fusion fascia of Toldt); 7, fourth part of duodenum; eight, left kidney parenchyma; 9, spleen. The fused right anterior perirenal fascia and right mesocolon (the fusion fascia of Toldt) is visible. Key: 1, thickened and infected retrocaecal appendix; 2, inflammatory fluid monitoring posteriorly in right pericolic house, anterior to proper perirenal house; three, anterior perirenal fascia (fused with retrocolic/mesocolic) fascia; four, caecum/ascending colon; 5, right kidney parenchyma; 6, right perirenal house 7, proper posterior pararenal space (the posterior perirenal fascia is troublesome to identify); 8, right quadratus lumborum; 9, right psoas main; 10, inferior vena cava; eleven, stomach aorta; 12, left psoas major; 13, left quadratus lumborum; 14, left erector spinae group; 15, left kidney parenchyma; sixteen, left posterior perirenal fascia; 17, left perirenal house; 18, left posterior pararenal house; 19, descending colon. Key: 1, thickened and inflamed retrocaecal appendix; 2, inflammatory fluid and oedema extending alongside right mesocolon in the direction of root of mesentery; 3, enlarged infected proper ileocolic lymph node; four, inflammatory fluid monitoring in right mesocolon; 5, inferior vena cava � retrohepatic section; 6, inferior vena cava � infrahepatic peritonealized segment; 7, inferior vena cava � renal section; eight, inferior vena cava � infrarenal segment; 9, left renal vein; 10, superior mesenteric artery; eleven, coeliac trunk; 12, belly aorta; 13, proper widespread iliac artery; 14, left frequent iliac artery (origin); 15, tail of pancreas. In the absence of a earlier surgical incision, herniation by way of the posterior stomach wall is rare as a outcome of the muscular and fascial layers usually defend towards protrusion of the posterior belly viscera, which are comparatively immobile. However, the posterior free border of exterior indirect, the inferior free border of latissimus dorsi, and the iliac crest delimit the lumbar triangle (of Petit), an space of potential weakness through which a lumbar hernia might develop (Stamatiou et al 2009). The mean adult infrarenal aortic diameter measured by computed tomography is 19�21 mm in males and 16�18 mm in women (Rogers et al 2013), however there are ethnic variations (Jasper et al 2014). The imply calibre of the abdominal aorta decreases barely from proximal to distal. A transverse part by way of the left renal hilum (the calculus is under the airplane of this section). Key: 1, left kidney parenchyma; 2, extravasated urine in left perirenal house; 3, posterior perirenal fascia; 4, anterior perirenal fascia (fused medially with retropancreatic fascia and fused laterally with proper leaf of descending mesocolon); 5, left posterior pararenal house; 6, descending colon; 7, third a half of duodenum; eight, inferior vena cava; 9, stomach aorta; 10, proper psoas main; 11, right quadratus lumborum; 12, proper erector spinae group; 13, aortocaval lymph node (borderline enlarged); 14, left para-aortic lymph nodes (borderline enlarged). Lumbar arteries come up from its dorsal aspect, and the third and fourth (and sometimes the second) left lumbar veins cross behind it to attain the inferior vena cava. On the right, the belly aorta is said superiorly to the cisterna chyli and thoracic duct, the azygos vein and the best crus of the diaphragm, which overlaps and separates it from the inferior vena cava and right coeliac ganglion. This close relationship permits the development of an aortocaval fistula, which is a uncommon complication of aneurysmal illness or trauma. On the left, the aorta is expounded superiorly to the left crus of the diaphragm and left coeliac ganglion. The anterior (unpaired) and lateral (paired) branches are distributed to the viscera, whereas the dorsal branches supply the physique wall, vertebral column, vertebral canal and its contents. Anterior group Coeliac trunk the coeliac trunk is the primary anterior department and arises just below the aortic hiatus, normally at the degree of the vertebral body of T12. It is 1�3 cm long and passes almost horizontally forwards and barely to the right above the physique of the pancreas and splenic vein.