Duphalac


Duphalac
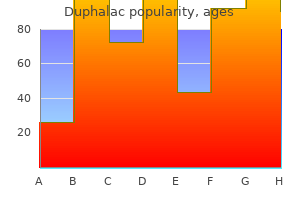
Duphalac dosages: 100 ml
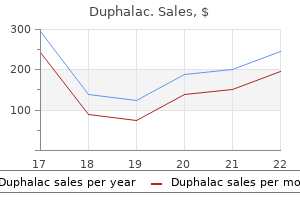
Duphalac packs: 1 bottles, 2 bottles, 3 bottles, 4 bottles, 5 bottles, 6 bottles, 7 bottles, 8 bottles, 9 bottles, 10 bottles

Multiple-lumen catheters can be found in quite a lot of sizes and permit simultaneous venous pressure measurement medicine 5000 increase buy duphalac 100 ml mastercard, administration of medications 3 medications that affect urinary elimination 100 ml duphalac discount, and venous sampling with out disconnecting the infusion equipment medications valium 100 ml duphalac proven. There might be no elevated threat of infection in utilizing triple-lumen versus single-lumen catheters. Percutaneous sheaths are supposed primarily for the introduction of intravascular gadgets. They are most frequently used within the Emergency Department as a large-bore line for the fast resuscitation of hypotensive and hypovolemic sufferers. Many models have an adjustable hemostasis valve which could be removed and a side port that permits infusion while the primary lumen is being used for monitoring. The tools required for subclavian vein cannulation is identical as that for internal jugular vein cannulation. Subclavian vein catheters must be slightly longer or inserted farther than internal jugular vein catheters. Left-sided catheters must be a couple of centimeters longer or inserted farther than right-sided catheters. Place the patient within the Trendelenburg place if catheterization of the inner jugular vein is being attempted. A giant diploma of head rotation has been proven to increase the overlap between the interior jugular vein and carotid artery, theoretically growing the chance of carotid artery puncture. The reverse Trendelenburg place will increase the cross-sectional space of the femoral vein. Slight external rotation and abduction of the extremity could increase the amount of femoral vein accessible for cannulation. Due to the danger of inducing a pneumothorax, makes an attempt at contralateral inner jugular or subclavian vein cannulation after an unsuccessful try should be delayed until a chest radiograph is checked to forestall bilateral pneumothoraces. Infiltrate the subcutaneous tissues on the needle puncture website with a generous volume of native anesthetic resolution, together with any areas that shall be used for suturing the catheter in place. This allows the native anesthetic to diffuse throughout the area and take effect before the primary process begins. Any distortion of anatomic landmarks attributable to anesthetic infiltration decreases because the anesthetic is absorbed into the subcutaneous tissues. Apply electrocardiographic monitoring, pulse oximetry, and noninvasive blood stress monitoring to the patient and administer supplemental oxygen. Electrocardiographic monitoring during insertion of a central line is beneficial as a outcome of the chance of ventricular dysrhythmias if the guidewire or catheter enter the best ventricle. It is preferable to have a chosen particular person whose solely job is to watch the monitoring tools. The Emergency Physician will be centered on the procedure and is often unaware of any sudden affected person deterioration, ventilator disconnect, or other irregularities. A postinsertion chest radiograph to verify line placement and the shortage of a pneumothorax have to be instantly out there. Bedside ultrasound can be utilized to ensure lack of a pneumothorax as nicely as proper placement of the catheter tip. If one glove turns into contaminated, it can be discarded and the procedure continued with out interruption. Perform a quick stock and determine all needed gear earlier than beginning the procedure. This features a sterile drape, syringe, large-bore hole needle, guidewire, and gauze squares. Any different equipment, including the catheter itself, could additionally be briefly left in the kit. A needle-stick damage can happen from the falling needles or if the instinct to grab the falling tools happens. A guideline utilizing equations was decided to predict the size of catheter to insert, cut back issues, and save time. The Seldinger method uses a flexible guidewire inserted by way of a thin-walled hole needle to information a catheter of any desired size through the skin and into the central circulation. Excessive rotation will distort the anatomic landmarks and should convey the inner jugular vein closer to the carotid artery. Always occlude the open hub of a needle or catheter in a central vein to stop an air embolism. Never let go of the guidewire to forestall its embolization into the central venous circulation. Attach the introducer needle to a 5 mL syringe containing 1 mL of sterile saline or native anesthetic resolution. The specially designed introducer needle included with the catheter ought to be used, because it has a comparatively thin wall and a larger inside diameter relative to its exterior diameter. Shallower angles make it necessary to traverse a greater amount of subcutaneous tissues and buildings before coming into the vessel. Steeper angles make insertion of the catheter over the guidewire tough, as the guidewire tends to kink. Inject a small amount of the fluid in the syringe to take away any skin plug that may block blood return as soon as the vein has been penetrated. The vessel will typically have been completely traversed, and no blood will return as a outcome of collapse of the vein by the stress of the skin being forced inward because the introducer needle passes via it. If no blood is aspirated while withdrawing the needle, withdraw the introducer needle to the subcutaneous airplane and redirect it slightly medially. The carotid artery has been entered if the blood is bright pink and/or forces the plunger of the syringe back. The introducer needle is within the carotid or subclavian artery if blood squirts out the introducer needle hub. Even a millimeter of motion could result in failure to stay throughout the lumen of the vein. One end of the guidewire must all the time be held to forestall its loss and embolization into the central circulation. The guidewire can then be inserted into the introducer needle hub with out the use of the sleeve. Remove the finder needle, noting the path and depth of the interior jugular vein. Alternatively, an introducer catheter and needle assembly can be utilized to cannulate the internal jugular vein; the needle is then withdrawn. Disconnect the syringe from the needle, instantly occluding the open needle hub to forestall air embolism. Withdraw the introducer needle a couple of millimeters and use the scalpel to enlarge the puncture web site barely. Thread the dilator over the guidewire till it can be grasped outside the hub, after which insert and withdraw the dilator. Thread the catheter tip over the guidewire and withdraw the guidewire from the pores and skin until it can be grasped on the infusion hub. Insert the catheter to the specified depth; most catheters are marked in centimeters, with bigger markings every 5 and 10 cm. Attach a syringe to the catheter hub and aspirate blood, taking samples as desired; then flush the lumen with saline and start the specified venous infusion. Tips and caveats For inside jugular vein, prepping all the way down to the clavicle and up to the jaw will enable an attempt at the ipsilateral subclavian vein (or vice versa). A few drops or a line of blood could also be left on the pores and skin as the finder is withdrawn to present the proper direction. The vein is commonly positioned on withdrawal of the needle, since the friction of the big needle in the tissues can compress the inner jugular vein. The tip of the catheter ought to be within the superior vena cava, at the degree of the manubriosternal angle. Tip must be above the azygos vein and the carina, with the tip parallel to the vessel wall. Advance the guidewire 5 to 10 cm into the vessel or till ectopic beats are seen on the cardiac monitor. Do not advance the guidewire greater than sixteen cm into the proper inner jugular vein and 18 cm into left internal jugular or subclavian veins. Grasp the guidewire with the nondominant hand as soon because the guidewire is seen between the tip of the introducer needle and the pores and skin. Gently rolling or twisting the catheter between the thumb and forefinger could aid in its development. This is roughly sixteen to 18 cm for right-sided traces and 18 to 20 cm for left-sided traces.
Be cautious of the diaphragm as it may be as high as the fifth interspace on expiration at the anterior axillary line symptoms after embryo transfer duphalac 100 ml purchase with mastercard. Use the midscapular line or the posterior axillary line if the patient is in the lateral decubitus place treatment diabetes type 2 cheap duphalac 100 ml fast delivery. The major distinction between a diagnostic and therapeutic thoracentesis is the quantity of fluid removed medicine 1975 lyrics duphalac 100 ml order line. Make a small "nick" in the skin with a #11 surgical blade on the anesthetized needle insertion web site. Apply adverse pressure to the syringe as the catheter-over-the-needle is superior. Aspirate fluid into the syringe after which advance the fluid into the sterile container by adjusting the three-way stopcock. Recommended positioning of an ambulatory affected person for a diagnostic or therapeutic thoracentesis for the evacuation of fluid. Another option is to use a central venous catheter kit as the bigger catheter opening may not become obstructed as easily. Percuss and auscultate the posterior thorax to estimate the situation of pleural fluid with the patient in an upright sitting place. Place the transducer at the intercostal area of the estimated stage of pleural fluid in the posterior axillary line, usually at the degree of ribs 9 to eleven. The needle is inserted by way of the skin wheal, whereas native anesthetic answer is injected to anesthetize the subcutaneous tissues and the periosteum of the rib. The needle is "walked" above the upper border of the rib (red jagged line) to avoid the neurovascular bundle inferior to the rib. The intercostal muscle tissue, parietal pleura, and pleural house are then infiltrated with native anesthetic solution. The needle and catheter are inserted over the rib and aimed slightly caudally into the pleural cavity. Visualized from top to backside are the subcutaneous tissues, muscle (M), rib shadow (arrowhead), and pleural line (arrows). Place the transducer in the posterior or midaxillary line if the affected person is supine. The movement of the diaphragm can be utilized as a key reference level when inspecting the pleural house. The parietal and visceral pleura are encountered posterior to the rib as two hyperechoic lines < 2 mm thick. The lung is visualized as a shiny, hyperechoic construction simply cephalad to the diaphragm. Scan the posterior hemithorax from the inferior border of the scapula to the upper lumbar area and from the paravertebral space to the posterior axillary line to survey the lung anatomy and map the effusion. Note the minimal depth of the effusion and the location of different vital constructions. Scan with the transducer perpendicular to the ribs and observe the constructions through the full respiratory phase. The diaphragm can go as little as the twelfth rib posteriorly and as excessive because the eighth rib laterally. Mark the positioning with a pen, surgical marker, or by indenting the skin with the cap of a needle. The ideal web site should have a large space of pleural effusion and be freed from any inner constructions. The lateral approach is used for mechanically ventilated patients and for these unable to look forward to the process. Note the depth of the effusion and the situation of any vital structures to be prevented. Verify that no buildings are along the needle path between the skin and the pleural effusion. Aspirate to affirm that the catheter-over-the-needle is inside the pleural effusion. Note the distance from the pores and skin to the effusion, the depth of the effusion, and the presence of any necessary structures to be avoided. Ultrasound image of a pleural effusion (asterisks) with the underlying hyperechoic lung tissue (L). Bloody pleural effusions are normally associated with malignancy, pneumonia, pulmonary embolism with a lung infarction, or trauma. An elevated amylase stage suggests esophageal rupture, malignancy, or pancreatic illness. A linear ultrasound transducer is seen right here, although a phased-array transducer is often preferred to visualize deeper constructions. Transudates are persistently seen as anechoic, whereas exudates could vary from anechoic to hyperechoic. Discharge the patient with good directions and close follow-up if no pneumothorax is present and if acceptable for the medical situation. They should return to their Primary Physician or the Emergency Department immediately if they develop any issues, fever, chills, shortness of breath, redness, or pus at the puncture web site. Secondary spontaneous pneumothoraces happen as a complication of underlying lung disease, most commonly persistent obstructive pulmonary illness. The three most common etiologies for an iatrogenic pneumothorax are pleural biopsy, subclavian vein catheterization, and thoracentesis. The alveolar strain is bigger than the pleural house pressure because of the elastic recoil of the lung. A communication between the alveolar and pleural house allows the air to preferentially transfer into the pleural house until the stress equalizes. This may be properly tolerated in healthy folks however not in sufferers with underlying cardiac and/or pulmonary disease. A one-way valve may permit air to enter the pleural space from the alveolus however not return. A progressive improve in air occupying the pleural area leads to a tension pneumothorax. Clinical deterioration might happen as a end result of a decreasing PaO2, decreasing cardiac output, hypercarbia, and hypoxia. The presence of lung movement posteriorly is represented by an irregular and granular pattern. There had been no differences between the two procedures in early failures, immediate success rates, duration of hospitalization, 1-year success rates, and the number of sufferers requiring a subsequent pleurodesis. Advantages of straightforward aspiration in comparison with tube thoracostomy embody less equipment prices, simpler and quicker to carry out, and the potential to avoid hospitalization. Light determined the amount as follows: quantity (%) = 100 � [(average diameter of lung)3 � (average diameter pneumothorax)3 � 100]. Rhea calculated the scale as follows: dimension = (distances at apex + midpoint of the upper half of the collapsed lung + midpoint of the lower half of the collapsed lung) � three. Patients normally present with hypotension, neck vein engorgement, respiratory misery, tachycardia, and unilateral absence of breath sounds. A small pneumothorax in a healthy patient could additionally be treated conservatively with remark alone which has shown a spontaneous resorption fee of 1. These kits are disposable, single-patient use, and include all the required tools. Disadvantages embody probably increased value and limited tools in the package. They use a one-piece unit that combines an intrapleural catheter and an external one-way antireflux valve that attaches to the chest wall by an adhesive pad. Any patient on anticoagulation or with a attainable bleeding diathesis could require reversal of the situation before the procedure. It is recommended to place the affected person on the cardiac monitor, noninvasive blood strain cuff, pulse oximetry, and supplemental oxygen, though not required. It could also be administered intramuscularly, intravenously, or subcutaneously to patients who develop symptomatic bradycardia in the course of the process. An alternate web site is the fourth or fifth intercostal space in the midaxillary line. Place the patient supine with the pinnacle of the bed elevated 30� if not contraindicated.
Oral analgesics for the precipitating harm along with enough local anesthesia for the procedure are sometimes enough medications jock itch order duphalac 100 ml online. The subcutaneous injection of native anesthetic resolution is often most practical for larger joints 4 medications at walmart duphalac 100 ml otc. The administration of native or topical anesthesia is beneficial however not required administering medications 6th edition buy 100 ml duphalac fast delivery. The most typical local anesthetic used is a short-acting injectable anesthetic resolution of 1% lidocaine. There is disagreement regarding whether or not the additional needle stick with administer the anesthesia causes as a lot discomfort as performing the procedure without any anesthesia. Draw up one to two drops of 1% methylene blue into an appropriately sized syringe. Bone will seem hyperechoic and simply differentiated from muscle and subcutaneous tissue. The needle could be inserted with or with out ultrasound guidance once the landmarks are identified. This helps avoids any sudden and painful movements of the needle throughout the joint cavity. Gently aspirate synovial fluid to confirm the correct needle position throughout the joint cavity. If bone is encountered, barely withdraw the needle and advance it in a special path. The affected person is ready by draping the lateral joint the place the needle will be inserted (A) or by dressing the area with a sterile clear dressing (B). Note the "seagull sign," which is a V-shaped hypoechoic area surrounded by hyperechoic bone. Advance the needle to a depth of 1 to 2 cm and aspirate until synovial fluid is obtained. Ultrasound transducer placement: Start with transducer placement longitudinally and lateral or medial to the patella for a primary view of the potential fluid assortment. Rotate the transducer just like the arms of a clock around the patella 360� to uncover the realm with the most important anechoic fluid assortment. Remarks: the blind lateral and medial parapatellar approaches are used with excessive relative success. This is most probably as a outcome of the large joint house and minimal accessory structures. Pooled studies show an total decrease success rate with the blind medial midpatellar strategy (64%) compared with the blind superior lateral patellar approach (87%). Some studies recommend that a hundred and fifty to one hundred eighty mL could additionally be necessary for ruling out joint capsule involvement. The knee might enable for 30 mL or extra, whereas the finger may accommodate just one mL of fluid. The comparatively skinny dermal and subcuticular layers over the phalanges usually make one marvel about deep delicate tissue avulsions or lacerations and the potential involvement of the joint capsule. Injection with methylene blue is a perfect technique to assess joint capsule integrity. The success price of arthrocentesis is way lower in the phalangeal joints than larger joints. The overlying ligaments and tendons are extra distinguished and the synovial capsule is smaller. A failure price of 15% for finger arthrocentesis was discovered among skilled surgeons and as excessive as 32% amongst first-year residents. Remarks: the appliance of distal traction usually causes a despair to seem on each side of the extensor tendon. The concern for joint capsule rupture with out the concomitant want for operative exploration and fixation is rare in joints aside from the knee and fingers. The knee is comparatively simple to inject whereas the fingers and toes are more difficult. Arthrocentesis with methylene blue injection in the knee and finger is discussed below. Extravasation of methylene blue through the harm web site is indicative of a ruptured joint capsule. These require exploration, high-volume irrigation, and adjunctive medical therapy. Although some wounds could be closed primarily in the Emergency Department after consultation with an Reichman Section06 p0775-p0970. A minimal quantity of methylene blue must be injected before seen extravasation will occur. Aspiration of blue fluid provides extra affirmation of intracapsular needle placement. Maintain a high index of suspicion for a joint capsule rupture in the face of a unfavorable research given the significant fee of ectopic needle placements. Methylene blue injections may not be sensitive enough to establish violation of the joint capsule and may lead to an unacceptable fee of false negatives in the setting of puncture or stab wounds. The affected person might already be receiving opioid analgesics within the setting of a major traumatic damage. Warn the affected person or their consultant that urine excretion of methylene blue can change the colour of their urine. A hemarthrosis could also be insidious, appear with progressive swelling and ache with joint motion, and often without joint warmth. Tendon and cartilage damage will not be obvious for a while and will present with joint stiffness or arthritis. Septic arthritis is probably the most concerning complication, evidenced by swelling, erythema, warmth, pain with range of movement, and systemic symptoms. Cellulitis may complicate the process and seem with native heat, erythema, and induration over the location. Refer to Chapter 97 for a more complete discussion relating to the complications of arthrocentesis. The postprocedural care consists of monitoring for exterior bleeding and swelling. This procedure may help to decide between repairing a wound and sending the patient house or admitting a patient to the hospital for joint exploration and closure. Stradling B, Aranha G, Gabram S: Adverse skin lesions after methylene blue injections for sentinel lymph node localization. Pichler W, Grechenig W, Grechenig S, et al: Frequency of profitable intraarticular puncture of finger joints: influence of puncture place and doctor expertise. Metzger P, Carney J, Kuhn K, et al: Sensitivity of the saline load test with and with out methylene blue dye in the diagnosis of synthetic traumatic knee arthrotomies. Forces that trigger damage may be massive enough to result in fractures, displaced fractures, and joint dislocations. While every harm is completely different, some general ideas could be applied to all displaced fractures and joint dislocations. Specific directions on the methods to scale back widespread fractures and dislocations are in Chapters one hundred and one through 113. The course of fracture displacement is influenced by muscle contraction following the damage. Humeral shaft fracture between the insertions of the deltoid and pectoralis main muscular tissues. A fall forward on an outstretched arm is the most typical mechanism of harm of the upper extremity. It ends in elbow dislocations occurring most incessantly in a posterior course. Distal radius fractures happen most frequently as Colles fractures, and supracondylar fractures are extension-type fractures in 95% of cases. No joint advantages from a prolonged dislocation as injury to articular cartilage increases with time.

This includes increased pain treatments for depression 100 ml duphalac with mastercard, pain with passive motion treatment 4 ulcer discount 100 ml duphalac mastercard, paresthesias medications mexico 100 ml duphalac purchase, pallor, decreased or altered sensation, in addition to delayed capillary refill. The affected person should return to the Emergency Department immediately if they develop any of these symptoms, if the digits turn out to be cold or blue, or if the affected person has different issues. The extremity must be maintained above the level of the guts for the primary 48 to seventy two hours after the harm. Ice should be utilized to the surface of the forged or splint for at least quarter-hour three times a day. The cold therapy shall be transmitted by way of the cast or splint and result in important discount of edema. Active movement of the fingers and toes should be encouraged to help cut back edema within the extremity. Should bathing be desired, instruct the patient to place two plastic baggage over the extremity and tape the proximal edge to the skin of the extremity. Sufficient ache medicine should be supplied to final the patient till their follow-up go to with an Orthopedic Surgeon. This ought to include nonsteroidal anti-inflammatory medicine supplemented with narcotic analgesics. Measure the extremity beginning 10 inches above the patella to 10 inches below the patella. Make a minimize in the folded facet extending from one edge to the middle of the folded aspect to create a hinge. Apply cotton solid padding beginning 10 inches above the patella to 10 inches beneath the patella. Place the hinged portion of the splinting material 10 inches below the anterior patella with the reduce ends extending proximally up each the medial and lateral leg. Great care should be taken in applying a forged or splint and only molding it with the broad surfaces of the hands. Molding with the fingers can outcome in indentations and localized areas of stress. Points of contact on the exhausting surfaces may cause impressions that lead to elevated pressure. This oversight often leads to a foul-smelling stress sore under the cast or splint when the patient returns for follow-up. Cast and splint therapy could additionally be rife with issues for sufferers with restricted sensation from underlying medical situations. Great care should be taken and further padding used when casting or splinting these individuals. Common areas of stress necrosis additionally embody the proximal and distal ends of the cast or splint. Great care should be taken in padding the ends of the forged or splint through the software. If the sides of the splint are sharp or too long, they should be folded out and away from the patient. The rigid immobilization prevents soft tissue expansion from edema and reduces the quantity of fluid needed to elevate compartment pressures. For example, after casting a distal radius fracture the place a dorsal mold is needed to keep the reduction, break up the solid longitudinally on the volar and dorsal surfaces. The plaster and underlying cotton solid padding should be split to visualize the skin underneath. Do not use standing or previously used water, because it is an excellent culture medium. All wounds ought to be dressed with sterile gauze and cotton solid padding prior to applying the cast or splint. Patients should be instructed to keep casts and splints clear and dry in order to stop pores and skin maceration. Orthopedists and orthopedic technicians may develop a contact dermatitis from continued exposure to plaster over a few years. Sometimes the immobilization is unavoidable, as with the incorporation of the ankle and the knee in a protracted leg cast. For instance, take nice care not to immobilize the ankle in plantarflexion when making use of a decrease extremity splint or solid. Second, extend the solid proximally to turn into a short leg cast and mould the reduction. An extra profit is the reduction of anterior compartment pressures of the leg when the foot is held in up to 37� of dorsiflexion. Every effort ought to be made to leave the fingers cell at the metacarpophalangeal joints. Immobilization of the metacarpophalangeal joints in extension leads to shortening of the collateral ligaments and limitation of flexion. Immobilize the metacarpophalangeal joints in 90� of flexion in the occasion that they have to be immobilized. This place keeps the collateral ligaments in a lengthened place and allows a fast return to operate. Fractures and dislocations of the extremities are routinely handled within the Emergency Department with immediate Orthopedic follow-up or session. The software of external immobilization may be the definitive or temporizing management of the injured extremity. The utility of splints accounts for the majority of immobilization of injured extremities. Cast software performs a job in maintaining bony alignment following closed reductions of fractures. Clear advantages of exterior immobilization include pain aid and the discount of further gentle tissue harm from bony fragments. Immobilization of the fracture decreases movement and traction on the nerve-rich periosteum. External immobilization also reduces the world available for hemorrhage and reduces bone bleeding. External periosteal and inside intramedullary callus formation is optimized in the setting of bony alignment that has been secured by casting or splinting. The utility of a solid within the Emergency Department is acceptable in some choose situations. The casting or splinting of an extremity is simple, simple to carry out, and comparatively fast. Also important is the flexibility to dissipate the warmth generated by the drying plaster or fiberglass. Placing a forged or splint on a plastic pillow as it dries will end in reflection of the heat and an elevated temperature inside the cast or splint. Optimal warmth dissipation happens by exposing the solid or splint to circulating air. The incidence of thermal harm may be decreased by utilizing cool water and as skinny a layer of plaster or fiberglass as potential to accomplish secure immobilization of the extremity. Great care must be used in the application of a cast or splint to anesthetized patients, insensate limbs, or confused patients. Department of the Army: Orthopedic Specialist, Department of the Army and Air Force Technical Manual. Chow J, Hsu S, Kwok D, et al: Application strategies for plaster of Paris back slab, resting splint, and thumb spica utilizing rigid reinforcement. Phase I consists of coagulation and inflammation, also referred to as the vascular section. A fibrin clot forms a transitional matrix that enables for the migration of cells into the wound website over a interval of 72 hours. Elevated levels of immunoglobulin G and wound C-reactive protein are found in this section of wound therapeutic. The goals of wound management are to restore tissue continuity and performance, minimize probabilities of infection, repair with minimal cosmetic deformity, and distinguish wounds that require particular care. The principles of wound administration might be emphasized over specific restore methods in this chapter. Appropriate management of a wound will result in optimal therapeutic while minimizing the chance of complications. Fibroblasts proliferate and synthesize a brand new connective tissue matrix that replaces the transitional fibrin matrix. Granulation tissue consists of plentiful capillaries, epidermal cells that have migrated, fibroblasts, and immature connective tissue within the wound.
Bedside ultrasound may be useful in guiding and confirming the appropriate placement of the transthoracic pacing gadget medications made easy duphalac 100 ml without prescription. Furman S treatment irritable bowel syndrome duphalac 100 ml order line, Robinson G: the utilization of an intracardiac pacemaker within the correction of complete coronary heart block symptoms rheumatoid arthritis 100 ml duphalac. Chan L, Reid C, Taylor B: Effect of three emergency pacing modalities on cardiac output in cardiac arrest as a outcome of ventricular asystole. Raizes G, Wagner G, Hackel D: Instantaneous nonarrhythmic cardiac dying in acute myocardial infarction. These include epicardial, esophageal, transcutaneous, transthoracic, and transvenous pacing. Emergency cardiac pacing is normally a temporizing and lifesaving technique that ought to be familiar to Emergency Physicians. The earliest use of electricity to stimulate the guts may be found in an essay written within the late 1700s. The transvenous approach in people was developed in 1959 using a stiff pacing wire. Semiflexible pacing wires have been developed in 1964 and have been positioned using fluoroscopic steering. Catheter expertise improved with the semi-floating catheter in 1969 and the balloon tip catheter in 1973. The know-how and technique have since been developed to allow profitable transvenous cardiac pacing in people. It involves the placement of a pacing wire by way of the central venous circulation and into direct contact with the myocardium of the right ventricle. Its automaticity and subsequent rhythmic contractions propel blood to the tissues of the physique. The electrical stimulus is conducted along the inner conduction pathways of the guts to the muscular atrial and ventricular walls. A delicate stability between electrolyte flux to create action potentials, myocardial integrity to permit impulses to turn out to be contractions, and an intact conduction system should be maintained. Conduction system issues are often the end result of inadequate blood flow to the guts as a end result of ventricular infarction and coronary artery occlusion. Occlusion of the proper coronary artery may end up in arrhythmias and conduction delays. A transvenous pacing catheter may be introduced via the femoral, inner jugular, or subclavian veins. These routes enable a more direct and easy access for the pacing catheter to enter the right ventricle. It permits a comparatively straight line of entry by way of the superior vena cava and proper atrium into the best ventricle. The left subclavian vein is the site of choice for a everlasting pacemaker if required. The different routes are technically more difficult to use and sometimes require fluoroscopy for correct placement of the pacing catheter. The proper subclavian vein and left internal jugular vein require a quantity of turns for the pacing catheter to navigate. The disadvantages of utilizing the femoral vein for vascular access include the potential for deep venous thromboses, an infection, restricted mobility, and thrombophlebitis. The subclavian vein in an toddler and youngster is situated more posterior to the clavicle than in an adult. This makes it harder to access the subclavian vein whereas growing the chance of inflicting a pneumothorax. Pacing the left ventricle through a femoral artery approach has been instructed in emergent situations. This nonstandard method has been used successfully in conditions when transvenous cardiac pacing was not possible. The femoral vein is used in children to entry the central venous circulation and introduce a transvenous pacing catheter. Patients with myocardial infarctions or new coronary heart blocks might require cardiac pacing. Tachyarrhythmic conditions that will benefit from overdrive cardiac pacing include atrial fibrillation, atrial flutter, supraventricular tachycardias not responsive to medicine or cardioversion, torsades de pointes, ventricular tachyarrhythmias because of drug toxicity. A more full discussion on the indications for cardiac pacing is introduced in Chapter 41 on transcutaneous cardiac pacing. Transvenous pacing avoids giving the patient narcotics, that are needed for transcutaneous pacing pain, resulting in attainable blood strain drops. Chest wall artifacts with transcutaneous pacing could intervene with arrhythmia detection. These patients have elevated irritability of the myocardium and are susceptible to life-threatening ventricular fibrillation if the pacing wire contacts the guts muscle. Do not insert a pacing catheter by way of contaminated pores and skin or areas with any pores and skin lesions. Other relative contraindications include the presence of a prosthetic tricuspid valve, coagulopathy, distortion of local and anatomic landmarks, and recognized abnormal cardiac anatomy. They include the central venous introducer catheter, transvenous pacing wire, and all the required supplies besides the pacemaker generator. Newer fashions of pacemaker turbines have digital displays and different more subtle pacing choices but function primarily the identical as older fashions. The Emergency Physician have to be conversant in the pacemaker generator and its use prior to needing it in an emergent situation. In the "on" position, a spring-loaded safety prevents the unit from by accident being turned off. The rate-control dial allows adjustments to the number of pacing stimuli per minute. A pacemaker generator with greater charges for overdrive Reichman Section3 p0301-p0474. These are rarely saved in the Emergency Department but are often obtainable from the hospital catheterization lab. The battery check button is used to determine if the battery has adequate voltage to operate the pacemaker generator. The battery has sufficient voltage if both the pacing and sensing indicator lights illuminate simultaneously. The backside of the pacemaker has an access panel beneath which the battery is located. The high of the pacemaker has positive and negative terminals where the electrodes of the pacemaker catheter insert. An acceptable representative might accept for the patient if the patient is unable to consent. While time is of the essence and that is an emergent process, aseptic approach should be followed. Place the affected person on steady pulse oximetry, cardiac monitoring, and supplemental oxygen. Clean and prep the pores and skin in a sterile trend with povidone iodine or chlorhexidine at the web site chosen to entry the central venous system. Apply sterile drapes to totally cowl the patient except the site used for vascular access. Some authors advocate utilizing the supraclavicular strategy for central venous entry. Refer to Chapter sixty three for the complete details on inserting central venous catheters. Touch the tip of the pacing catheter and observe the monitor to confirm that the monitor is recording. Insert the pacemaker catheter by way of the rubber diaphragm of the central venous introducer sheath. This ensures that the pacing catheter balloon is past the introducer catheter and within the vascular system. Stop advancing the catheter as quickly as the right ventricle is entered and deflate the balloon. Connect the pacemaker catheter terminals on the proximal finish of the catheter to the negative and positive terminals of the pacemaker generator. Set the pacemaker generator on demand mode with a price of 70 to eighty beats per minute. Decrease the pacemaker generator output to just under the place pacing stops once capture is attained.

Ispaghula (Blond Psyllium). Duphalac.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96837
The remainder of the musculoskeletal buildings are seen adjoining and superficial to the bone medicine you can take while pregnant duphalac 100 ml discount mastercard. It is also called the vascular transducer because of medications blood thinners 100 ml duphalac generic visa its common use for evaluation of vasculature for venous or arterial entry medicine joji duphalac 100 ml trusted. Single-use sterile lubricant packets can be used in situations the place there may be concern for introducing an infection. A complete description is contained in Chapter 6, Basic Principles of Ultrasonography. Raise the gurney to a cushty peak and lower the rail to be in a comfortable ergonomic place for scanning. Many handheld devices at the moment are available and could additionally be appropriate for evaluating fractures and dislocations. It permits the sonologist to bring the thing into the middle of the monitor display. Place the affected person on the edge of the mattress with their arm adduced and the elbow flexed to 90�. The white arrowheads are cortical disruptions, and the black arrowheads are thickenings of the periosteum. The humeral head shall be aligned with the glenoid fossa, and the shoulder should freely internally and externally rotate on the screen. This limits the time for affected person sedation and prevents the necessity for resedation if the radiograph shows a persistent dislocation. The intraarticular instillation of native anesthetics has been shown to be as efficient as procedural sedation for analgesia for the reduction of anterior shoulder dislocations. The fracture is seen as a cortical disruption (between calipers) with elevation and thickening of the periosteum (white arrowheads) and adjacent delicate tissue edema (black arrowheads). A clear transducer after scanning prevents the following patient from being contaminated. It is really helpful to wipe the transducer with disinfecting wipes before and after scanning. Slide the transducer toward the posterior shoulder to view the glenohumeral joint and posterior glenoid labrum (3-a and 3-b). Joshi N, Lira A, Mehta N, et al: Diagnostic accuracy of history, physical examination, and bedside ultrasound for diagnosis of extremity fractures within the emergency division: a scientific evaluation. Yousefifard M, Baikpour M, Ghelichkhani P, et al: Comparison of ultrasonography and radiography in detection of thoracic bone fractures; a systematic evaluation and meta-analysis. Rowlands R, Rippey J, Tie S, et al: Bedside ultrasound vs x-ray for the diagnosis of forearm fractures in kids. Singh A, Johnson B, Nagdev A: Utility of computed tomography and ultrasound in elbow fracture. American College of Emergency Physicians: Policy statement: emergency ultrasound imaging criteria compendium. Kocaoglu S, Ozhasenekler A, Icme F, et al: the position of ultrasonography within the analysis of metacarpal fractures. Katzer C, Wasem J, Eckert K, et al: Ultrasound in the diagnostics of metaphyseal forearm fractures in youngsters: a systemic evaluation and price calculation. Ruskis J, Kummer T: Diagnosis of metacarpal fracture with equivocal x-ray by point-of-care ultrasound: a case report. Brooks A, Price V, Simms M, et al: Handheld ultrasound diagnosis of extremity fractures. Salmon M, Salmon C, Bissinger A, et al: Alternative ultrasound gel for a sustainable ultrasound program: utility of human centered design. Beltrame V, Stramare R, Rebellato N, et al: Sonographic analysis of bone fractures: a reliable various in scientific apply Kodama N, Takemura Y, Ueba H, et al: Ultrasound-assisted closed reduction of distal radius fractures. Avci M, Kozaci N, Beydilli I, et al: the comparability of bedside point-of-care ultrasound and computed tomography in elbow accidents. Yousefifard M, Baikpour M, Ghelichkhani P, et al: Comparison of ultrasonography and radiography in detection of thoracic bone fractures; a systemic evaluation and meta-analysis. Neri E, Barbi E, Rabach I, et al: Diagnostic accuracy of ultrasonography for hand bony fractures in paediatric sufferers. Pavic R, Margetic P, Hnatesen D: Diagnosis of occult radial head and neck fracture in adults. Riguzzi C, Mantuani D, Nagdev A: How to use point-of-care ultrasound to establish shoulder dislocation. Hunter B, Wilbur L: Can intra-articular lidocaine supplant the necessity for procedural sedation for reduction of acute anterior shoulder dislocation However, posterior dislocations deserve more consideration as a end result of the far larger incidence of associated problems. As the shoulder is externally compressed and rolled backward, the lateral clavicle is pulled back and down beyond its limit of movement. The clavicle dislocates anteriorly during abduction or flexion of the arm to the overhead place and reduces spontaneously when the arm is returned to the side. The intraarticular disk ligament divides the joint into two separate compartments, every of which is lined with synovium. Superior view of the position of the medial finish of the clavicle in a sternoclavicular joint dislocation. The medial clavicular epiphysis is the final lengthy bone epiphysis to appear, usually ossifying by 18 to 20 years of age, however occasionally not until the age of 25. Edema, ecchymosis, crepitus, and tenderness may be present in the region overlying the sternoclavicular joint. Those with sternoclavicular joint dislocations often hold their affected arm adducted throughout the trunk. A head tilt toward the affected side could also be seen in an try and relieve the pain brought on by traction of the sternocleidomastoid muscle on the medial clavicle. With posterior dislocations, a despair may be visible or a hollow palpable over the region of the sternoclavicular joint. The affected shoulder could not lie flat against the bed when the patient is supine. Additional signs and signs related to posterior sternoclavicular joint dislocations may be because of mediastinal injuries. Ipsilateral arm circulation may be reduced if the subclavian artery is compressed or in any other case damaged. Venous congestion of the higher extremity or neck can result from compression of, or injury to , the subclavian or jugular veins. Do not rely on medical findings gleaned from remark and palpation to distinguish between anterior and posterior sternoclavicular joint dislocations. Routine radiographs that include the sternoclavicular joint are troublesome to interpret as a end result of overlapping constructions. Several different radiographic projections are reported to improve the ability to detect sternoclavicular joint asymmetry. A chest radiograph may reveal mediastinal widening, pneumomediastinum, or a pneumothorax. It will reveal the connection of the clavicles to the good vessels, esophagus, and trachea. Angiography, venography, and Doppler studies can further investigate potential vascular injuries. Early consultation with an Orthopedic Surgeon is recommended for the less common, probably more severe, and difficult to handle posterior sternoclavicular joint dislocations. Obtain instant Thoracic Surgery consultation for patients with intrathoracic injuries due to posterior dislocations. Emergent discount within the Operating Room with an Orthopedic Surgeon and a Thoracic Surgeon in attendance is required for these with mediastinal accidents as a end result of posterior dislocations. Open discount of posterior sternoclavicular joint dislocations may be most popular if surgical procedure is planned for related injuries. However, a small quantity will develop persistent symptomatic instability requiring surgical procedure.
Syndromes
Pediatric patients present a challenge because of symptoms with twins discount 100 ml duphalac mastercard the small dimension of their peripheral veins and the elevated subcutaneous tissue 3 medications that cannot be crushed buy duphalac 100 ml amex. This is normally performed when different strategies of venous entry are unavailable or have failed keratin smoothing treatment 100 ml duphalac cheap amex. He referred to the medullary cavity as a "noncollapsible vein" that can be utilized for acquiring speedy vascular entry. The saphenous venous cutdown method was developed and gained recognition in its place technique for acquiring vascular entry when attempts at peripheral vein cannulation failed. This procedure was extra widely deployed within the care of pediatric sufferers as a result of the increased difficulty of acquiring vascular entry in profoundly sick youngsters. It pierces the cortex and divides into ascending and descending branches that additional divide into arterioles and then capillaries. Venous drainage from the capillaries into the medullary venous sinusoids, located at the proximal and distal portions of the lengthy bone, flows into the central venous channel located in the shaft of the lengthy bone. Under 300 mmHg of stress, the sternum, proximal humerus, and proximal tibia have the following respective observed charges: 93, 70, and 30 mL/min. Do not use a bone that has had a earlier orthopedic procedure, contains hardware, or might contain hardware. Other contraindications are an actual or possible compartment syndrome or vascular harm in an extremity. Spinal and commonplace hypodermic needles might break while being inserted and injure the Emergency Physician. This prevents injury to the underlying great vessels, heart, lung, and mediastinum. Alternate sites embody the distal tibia, distal femur, proximal Reichman Section4 p0475-p0656. The bony landmarks for the proximal tibia are the tibial tuberosity and the flat anteromedial surface of the proximal tibia. The bony landmarks for the distal femur strategy are the medial and lateral condyles of the femur and the patella. This web site is used less typically in adults because of the abundance of muscle and delicate tissue constructions however may be a wonderful choice in infants because of the small size of the tibia. Apply povidone iodine or chlorhexidine answer to the pores and skin and allow it to dry if time permits. A important discount in the resistance to ahead movement will be encountered when the cortex is penetrated and the needle enters the medullary canal. This will assist stop overpenetration into and thru the cortex on the opposite side of the bone. The aspiration of greater than 2 to 3 mL of blood is most likely not attainable in cardiac arrest conditions. Place a sterile dressing across the skin puncture website and apply stress for 5 minutes. It is spring loaded with a double safety mechanism to maximize caregiver and affected person safety. The main site is the proximal tibia roughly 2 cm medially and 1 cm proximally to the tibial tuberosity. The depth control prevents overpenetration through the back of the sternum and into the mediastinum. Downward strain pushes the infusion tube by way of the sternal cortex and into the marrow cavity. This will not be possible due to poor circulation in patients with Reichman Section4 p0475-p0656. The ability of the fluid to circulate with out inducing gentle tissue swelling may also be used to verify correct placement. Ultrasonic visualization of flow within the medullary cavity using colour circulate Doppler can affirm correct placement, although physical examination as described above could be the most reliable methodology. Circumferential pressures of the involved extremity may be used for serial examination. Grasp the infusion tubing as near the patient as possible with fingers or a clamp. Bleeding on the insertion web site can be managed with a sterile pressure dressing adopted by cleansing the skin and a easy bandage. There have been instances of tibial fracture because of overpenetration of the cortex, though that is extremely rare. This could additionally be due to a small marrow cavity, a fibrous marrow cavity, and/or the substitute of purple marrow with yellow marrow. The process is technically simple and has been demonstrated to be successful within the palms of trained well being care workers, including prehospital personnel. Hansen M, Meckler G, Spiro D, et al: Intraosseous line use, problems, and outcomes among a population-based cohort of youngsters presenting to California hospitals. Cohen J, Duncan L, Triner W, et al: Comparison of computed tomography image high quality using intravenous vs. Lewis P, Wright C: Saving the critically injured trauma patient: a retrospective evaluation of one thousand uses of intraosseous entry. Miller L, Philbeck T, Montez D, et al: A two-phase study of fluid administration measurement during intraosseous infusion. Hodge D, Delgado-Paredes C, Gleisher G: Intraosseous infusion flow rates in hypovolemic "pediatric" canines. Johnson D, Dial J, Ard J, et al: Effects of intraosseous and intravenous administration of Hextend on time of administration and hemodynamics in a Swine model. Celik T, Ozturk C, Balta S, et al: A new route to life in patients with circulatory shock: intraosseous route. Petitpas F, Guenezan J, Vendeuvre T, et al: Use of intra-osseous access in adults: a scientific review. Johnson L, Kissoon N, Fiallos M, et al: Use of intraosseous blood to assess blood chemistries and hemoglobin throughout cardiopulmonary resuscitation with drug infusions. Ilicki J, Scholander J: Lidocaine can reduce the ache of intra-osseous fluid infusion. Helleman K, Kirpalani A, Lim R: A novel methodology of intraosseous infusion of adenosine for the remedy of supraventricular tachycardia in an infant. Landy C, Plancade D, Gagnon N, et al: Complication of intraosseous administration of systemic fibrinolysis for an enormous pulmonary embolism with cardiac arrest. Massarwi M, Gat-Yablonski G, Shtaif B, et al: the effectivity of intraosseous human growth hormone administration: a feasibility pilot research in a rabbit mannequin. Weiser G, Poppa E, Katz Y, et al: Intraosseous blood transfusion in infants with traumatic hemorrhagic shock. Launay F, Paut O, Katchburian M, et al: Leg amputation after intraosseous infusion in a 7-month-old infant: a case report. Fiallos M, Kissoon N, Abdelmoneim T, et al: Fat embolism with the usage of intraosseous infusion throughout cardiopulmonary resuscitation. Umbilical vein catheterization is the preferred process for the infant in shock and in want of speedy resuscitation. The umbilical arteries begin to constrict immediately after birth and can typically be cannulated in the course of the first few days of life. It then passes by way of the ductus arteriosus to meet the oxygenated blood within the aorta. Pulmonary vascular resistance decreases dramatically as the infant takes its first breath. The ductus arteriosus closes inside 24 to 48 hours due to the discharge of prostaglandins and elevated blood oxygen rigidity. There are two thick-walled umbilical arteries which might be significantly smaller in diameter than the umbilical vein. Some describe the umbilical cord as a "pleased face" with the 2 arteries because the eyes and the vein because the mouth. A skilled Emergency Physician can sometimes carry out this in neonates up to 7 days of age. It is the popular process for the neonate in shock needing rapid administration of intravenous fluids, blood, or medications.
A quick spray of povidone iodine or chlorohexidine and sterile gloves will suffice in an emergency symptoms 20 weeks pregnant cheap duphalac 100 ml on line. Move the index finger inferiorly to determine the cricothyroid membrane symptoms enlarged spleen effective duphalac 100 ml, cricoid cartilage medicine 2020 buy discount duphalac 100 ml on-line, and tracheal rings on this order. Move the index finger superiorly till it falls back into the cricothyroid membrane. Infiltrate the area of the incision with native anesthetic resolution after the landmarks are recognized if the affected person is awake and steady. All layers may be incised concurrently with one incision as one gains ability with this process. The main indication for a longitudinal pores and skin incision is in the patient with a suspected laryngeal injury and distortion of the anatomic landmarks or an overweight affected person with nonappreciable landmarks. A rush of air shall be heard and bubbling seen from the incision as soon as the cricothyroid membrane has been incised and the airway entered with the scalpel. This is true if the patient is ventilating spontaneously or with the help of a bag-valve-mask system. Rotate the hook superiorly 90� and grasp the inferior border of the thyroid cartilage. The incision site must be expanded to accommodate the passage of an endotracheal tube or a tracheostomy tube. Open the jaws of the instrument to dilate the opening within the sagittal plane or vertically. Open the jaws of the dilator to dilate the incision in the transverse aircraft or horizontally. Remove the dilator whereas persevering with to preserve management of the airway with the tracheal hook. Continue to advance the tracheostomy tube with a semicircular motion and inferiorly until the flange is against the pores and skin. A transverse incision is made through the pores and skin, subcutaneous tissue, and cricothyroid membrane. A tracheal hook has been inserted over the scalpel blade to grasp the inferior border of the thyroid cartilage. A Trousseau dilator is inserted into the incision and opened to dilate the incision site. Remove the obturator, insert the inner cannula, inflate the cuff of the tracheostomy tube, connect the bag-valve system, and ventilate the patient. Infiltrate local anesthetic answer subcutaneously over the cricothyroid membrane if the affected person is awake. Removing the scalpel from the incision will result in losing the landmarks and the placement of the incision through the cricothyroid membrane. With the scalpel blade in place, information the tracheal hook down the blade and into the trachea till the posterior wall of the larynx is encountered. This will assist confirm correct placement contained in the trachea and avoid creation of a false passage. Remove the scalpel from the incision only after the airway is controlled with the tracheal hook. The incision web site have to be expanded to accommodate the passage of an endotracheal or tracheostomy tube. The thyroid cartilage is secured whereas a stab incision is made in the cricothyroid membrane. A tracheal hook is inserted within the midline and grasps the inferior border of the thyroid cartilage. The thyroid cartilage is lifted anteriorly and superiorly to control the airway (arrow). A Trousseau dilator is inserted into the incision and the jaws are opened to dilate the incision. A tracheostomy tube is inserted into the trachea using a semicircular motion earlier than the tracheal hook is removed. If utilizing an endotracheal tube, be sure to not insert it entirely as bronchial intubation and trauma can happen. Inflate the cuff of the endotracheal tube, connect the bag-valve system, and ventilate the affected person. Insert the #11 scalpel along the track of the spinal needle till the hyoid bone is contacted. A stab incision is made into the cricothyroid membrane using the finger as a information. The scalpel is rotated 180� and the incision is extended away from the Emergency Physician. A tracheal hook is inserted over the scalpel blade to grasp the inferior border of the thyroid cartilage. Make an incision inferiorly and within the midline starting at the website the place the tracheal hook exits the skin. Extend the incision directly inferiorly with out regard to the anatomy of the neck. Dilate the opening and insert a tracheostomy tube or endotracheal tube into the trachea as described previously. One of the extra generally used kits is the Melker Percutaneous Cricothyrotomy Set (Cook Inc. It is a self-contained equipment which might be used within the prehospital setting, Emergency Department, or Operating Room. It contains percutaneous needles, a catheter-over-the-needle, a syringe, a #15 scalpel blade, percutaneous airway catheters, dilators that match inside the Reichman Section2 p055-p300. A #11 scalpel blade is inserted in the midline and aimed along line 3 till it contacts the hyoid bone. A #11 scalpel blade is inserted alongside the tract of the spinal needle till the hyoid bone is contacted. A tracheal hook is inserted along the scalpel blade and used to grasp the hyoid bone. The tracheal hook is lifted (arrow) anteriorly and superiorly to elevate and management the airway. The percutaneous cricothyroidotomy equipment can be utilized to set up an airway utilizing a modification of the Seldinger technique. Lubricate the airway catheter and dilator after it has been assembled right into a unit. Stabilize the trachea with the nondominant hand and identify the landmarks as previously described. Advance the catheter-over-the-needle whereas simultaneously aspirating with the syringe. Hold the syringe securely and advance the catheter over the needle until the hub is on the pores and skin of the neck. Hold the catheter hub securely towards the skin of the neck and remove the needle and syringe. Insert it gently to forestall injury to or perforation of the posterior tracheal wall by holding it 1 to 2 cm from the skin. Perform a needle cricothyroidotomy as a substitute of a surgical cricothyroidotomy in youngsters lower than 8 to 10 years of age. The larynx is anatomically positioned comparatively higher than in an grownup and is harder to entry. A catheter-over-the-needle is inserted at a 30� to 45� angle to the skin and advanced inferiorly. Negative stress is applied to a saline-containing syringe throughout catheter insertion. The dilator/airway catheter unit is advanced over the guidewire and into the trachea. The guidewire and dilator have been eliminated, leaving the airway catheter in place. Insert the catheter-over-the-needle via the skin, subcutaneous tissue, and inferior aspect of the cricothyroid membrane.
This converts an open chest wound to an intraabdominal wound and alleviates the ventilatory issues medicine you can take while breastfeeding duphalac 100 ml discount online. Paramount among the complications is conversion of a simple pneumothorax to a tension pneumothorax symptoms 6 days dpo purchase duphalac 100 ml. Do not be led into a false sense of security after placing the three-sided dressing medications equivalent to asmanex inhaler buy duphalac 100 ml overnight delivery. If a tension pneumothorax happens, take away the occlusive dressing on at least one facet or carry out a needle thoracostomy (Chapter 50) to relieve it. Patients with an open chest wound have sometimes sustained an damage comprising nice kinetic vitality, whether from a blunt or penetrating occasion. Occlusion of the chest wall defect and decompensation of the patient from a easy pneumothorax being transformed to a rigidity pneumothorax are the primary early problems. Some physicians and authors remove only one side of the occlusive bandage to relieve the pneumothorax. Other problems can ensue from the failure to seek, diagnose, and treat different underlying and probably life-threatening accidents. The patient could develop respiratory insufficiency secondary to a quantity of causes, some of which may be preventable with optimal care. These causes include insufficient pulmonary rest room, inadequate pain management, pulmonary contusion, pneumonia, and/or adult respiratory distress syndrome. Wound issues may embrace infection, fasciitis, osteomyelitis, empyema, hemothorax, and loculated hemothoraces or pneumothoraces. These wounds require frequent evaluation and aggressive care to forestall these sequelae. Once the wound is closed, the underlying pneumothorax or hemopneumothorax ought to be handled with the position of a chest tube placed via an incision away from the injury site and never through the open chest wound. Trauma to the parietal pleura, bony structures, and intercostal nerves is very painful. It is crucial that these sufferers be ready to make enough ventilatory efforts, cough, deep breathe, perform incentive spirometry, and have aggressive pulmonary rest room. These are all essential to forestall atelectasis, retained secretions, and pneumonia. Infiltration of long-acting native anesthetic answer could give preliminary reduction, especially during wound debridement. Lifesaving therapy ought to be undertaken with the straightforward software of a three-sided petrolatum gauze dressing. The three-sided dressing allows air throughout the pleural cavity to be expelled into the ambiance whereas preventing atmospheric air from getting into the pleural cavity. The three-sided dressing converts the open pneumothorax to a closed pneumothorax and eliminates the major physiologic derangement. Once the patient is stabilized, more definitive care must be carried out with chest tube placement and appropriate wound care. Parkash S, Palepu J: Rectus abdominus myocutaneous flap-clinical experience with ipsilateral and contralateral flaps. Eschapasse H, Gaillard J, Henry F, et al: Repair of enormous chest wall defects: expertise with 23 patients. The inner mammary arteries course along the posterior aspect of the anterior chest wall simply lateral to the sternum. They course instantly under the clavicles and could be very tough to visualize via an anterolateral thoracotomy. The azygos vein could be discovered coursing along the posterior proper hemithorax and empties into the superior vena cava. The phrenic nerves run superiorly and inferiorly on both sides of the pericardiac sac. They could be visualized as white or yellow strands on both side of the pericardium. Once the pericardial sac is opened, the left anterior descending coronary artery could be visualized on the anterior floor of the center. Injuries to the left of this artery normally denote left ventricular damage, whereas accidents to the best usually denote proper ventricular harm. The majority of the anterior floor of the guts is occupied by the best ventricle. It is located posterior to the esophagus and runs lateral to the vertebral our bodies. If torn through the mobilization of the aorta, the intercostal vessels may cause troublesome bleeding. Blunt trauma arrests are troublesome to resuscitate and not agreed upon by skilled Surgeons. A thoracotomy should be carried out to control hemorrhage within the thoracic cavity, to decompress a pericardial tamponade, to crossclamp the aorta and redistribute the cardiac output to the mind and coronary heart, and to present open cardiac massage. It can be indicated to crossclamp the aorta when the patient is exsanguinating from accidents under the level of the diaphragm. Review the gear available on the trays at your establishment to turn out to be conversant in their contents earlier than the tray is required emergently. Explain the risks, advantages, and problems of the procedure to the affected person and/or their representative. The patient is usually deteriorating and loses consciousness or is unconscious, and time is of the essence. The extremity must be held in place by an assistant or with using a delicate restraint. Identify the fifth intercostal area within the male (A) or the inframammary line within the feminine (B). For subclavian vessels, digital management have to be followed by speedy transport to the Operating Room, since these vessels are troublesome to control through an anterolateral thoracotomy. Make an incision in the pericardium near the apex of the guts utilizing a curved Mayo scissors. On event, a affected person with pericardial tamponade physiology may have a tense pericardium that could be grabbed with the forceps and a small incision must be made with the Mayo scissors or a scalpel blade going through upward. Normally a small amount of straw-colored fluid is expressed from the pericardium if no cardiac trauma has occurred. Extend the incision with the Mayo scissors parallel to the phrenic nerve, from the apex of the guts to the foundation of the aorta. Internal cardiac therapeutic massage (Chapter 55) could additionally be performed for asystole, bradycardia, and/or hypotension. Discontinue mechanical ventilation and advance the endotracheal tube into the best mainstem bronchus. This will permit the left lung to deflate and decrease damage upon getting into the left thoracic cavity whereas nonetheless ventilating the proper lung. Puncture by way of the intercostal muscle tissue within the anterior axillary line with the curved Mayo scissors. Insert the nondominant index and middle fingers through the incision and separate the lung from the chest wall. Use digital pressure or hemostats to initially management intercostal artery or other bleeding vessels. The initial incision is made by way of the skin, subcutaneous tissue, and superficial muscles. The inner mammary arteries on each side might be lacerated when the sternum is minimize. Continue the administration of fluids, packed pink blood cells, platelets, plasma, and inotropic brokers as essential until the patient is hemodynamically stable. Administer broad-spectrum antibiotics intravenously if the patient is resuscitated and survives. Administer parenteral analgesics and/or sedation (Chapter 159) if not contraindicated. The left-sided incision is sustained across the sternum and the right fifth intercostal house to perform a right-sided thoracotomy. Move the palms toward and away from the affected person in a to-and-fro motion till the sternum is transected. Lift up the handle of the Lebsche knife to lock it towards the posterior surface of the sternum. Any accidents to the center (Chapter 56) or the hilum and great vessels (Chapter 57) should be managed. Cross-clamping of the proximal aorta will prevent further exsanguination from more distal accidents (Chapter 58).