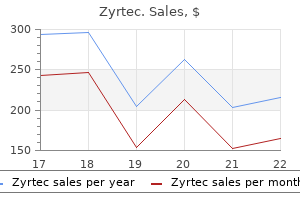
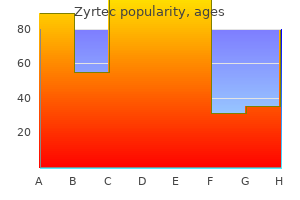
Zyrtec
Zyrtec
Zyrtec dosages: 10 mg, 5 mg
Zyrtec packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Following such therapy allergy medicine diphenhydramine zyrtec 10 mg cheap line, sufferers typically should continue acidsuppression therapy due to persistent allergy research group buy cheap zyrtec 10 mg line, although typically less severe allergy medicine zyrtec d zyrtec 10 mg buy fast delivery, symptoms. In a affected person with a hiatal hernia, the hernia is reduced again into the stomach during surgery. Gastroesophageal Reflux Disease 13 these procedures are most frequently accomplished laparoscopically to cut back the length of hospital stay and operative morbidity. Half of all patients who endure fundoplication still require acidsuppression medication. Most sufferers have gentle or moderate signs that reply to life-style modifications and antacid remedy. However, some sufferers have severe daily, as nicely as nighttime, symptoms that may considerably scale back their quality of life. In patients with atypical or refractory symptoms, ambulatory pH testing and, in some circumstances, impedance testing are useful in determining whether or not the signs are truly associated to gastroesophageal reflux. Questions Questions 1 and 2 relate to the scientific vignette discussed initially of this chapter. Gastroesophageal Reflux Disease 15 2 Six months later, the patient reviews intermittent issue swallowing stable food corresponding to bread or rice. Achalasia is a motility dysfunction of the esophagus that presents with progressive dysphagia for both solids and liquids. He has no issue swallowing liquids, and denies odynophagia, choking, cough, or shortness of breath. Physical examination reveals a wellnourished, middleaged man with a blood stress of 128/88 mmHg, pulse price seventy two per minute, temperature 98. When asked to swallow a sip of water, he swallows normally without choking or coughing. Routine laboratory exams show a normal full blood depend and complete metabolic panel. The situation outcomes from impeded transport of liquids, solids, or each, from the pharynx to the abdomen. Odynophagia refers to ache during swallowing and is incessantly associated with dysphagia. Swallowing issues can occur in all age groups, however the frequency of dysphagia is larger in the elderly. From 7�10% of adults older than 50 years of age, up to 25% of hospitalized patients, and 30�40% of nursing house residents experience issues with swallowing. Oropharyngeal dysphagia, or switch dysphagia, refers to difficulty transferring food (solids, liquids, or both) from the oropharynx to the esophagus. Esophageal dysphagia refers to difficulty passing meals via the esophagus into the stomach. The process of swallowing sometimes is divided into three distinct phases: oral; pharyngeal; and esophageal. The oral part includes preparing and propelling the food from the anterior oral cavity into the oropharynx, where an involuntary swallowing reflex is initiated. The diagram exhibits the switch of a bolus of food from the mouth (a) to the oropharynx (b) to the higher esophagus (c). Dysphagia 21 the oral part is the only voluntary part of swallowing and requires coordinated contractions of the tongue and striated muscular tissues of mastication. The pharyngeal section involves overlapping occasions that are critical to defend the airway whereas allowing the bolus to transfer to the esophagus. The meals bolus is propelled into the pharyngeal cavity, whereas the soft palate elevates and closes the nasal aperture and the larynx begins to elevate. The larynx closes and the soft palate and the posterior pharyngeal wall oppose the posterior aspect of the tongue to forestall reflux of food into the oral cavity. The final step includes opening of the upper esophageal sphincter to enable the passage of meals to the esophageal lumen. In the esophageal part, the food bolus is propelled down the esophagus by peristaltic contractions. This is accompanied by a relaxation of the lower esophageal sphincter and emptying of the esophageal contents into the gastric lumen. Etiology Oropharyngeal Dysphagia Oropharyngeal dysphagia could be attributable to mechanical obstruction or neuromuscular disease (Table 2. Stroke is the most common explanation for oropharyngeal dysphagia within the inpatient setting. Mechanical Obstruction the commonest reason for esophageal dysphagia is mechanical obstruction of the esophageal lumen (Table 2. Dysphagia usually happens when the diameter of the esophageal lumen is thirteen mm or less. Patients might have threat factors such as smoking and alcohol use within the case of squamous cell carcinoma, or longstanding gastroesophageal reflux disease within the case of adenocarcimona. Mechanical obstruction Intrinsic narrowing: Benign strictures: gastroesophageal reflux disease, caustic substances, medicines, postsurgical, radiation remedy Cricopharyngeal hyperplasia/bar Esophagitis: infectious, eosinophilic, pillinduced; gastroesophageal reflux illness Esophageal rings and webs Esophageal diverticula Tumors: benign or malignant Extrinsic compression: Anterior mediastinal mass Vascular lesions: � Congenital: aberrant right subclavian artery (dysphagia lusoria), rightsided aorta � Acquired: aortic aneurysm, left atrial enlargement, rightsided aorta Esophageal motility disorders Achalasia Distal esophageal spasm Hypertensive peristalsis (jackhammer esophagus) Hypotensive peristalsis (scleroderma) Esophageal stricture: esophageal strictures could be caused by caustic ingestion, sure drugs, gastroesophageal reflux illness, and radiation remedy. Esophageal rings and webs: rings or webs typically cause intermittent nonprogressive dysphagia. Esophagitis: dysphagia attributable to esophagitis is often accompanied by odynophagia. Medications identified to trigger esophagitis embody aspirin and different nonsteroidal antiinflammatory medicine, doxycycline or tetracycline, bisphosphonates, and potassium preparations. Eosinophilic esophagitis is a situation during which the esophageal mucosa is abnormally infiltrated with eosinophils. It is essential to rule out eosinophilic esophagitis in patients with dysphagia and a normal upper endoscopy; therefore, an esophageal biopsy is always recommended in such patients, and usually leads to intermittent dysphagia and meals bolus impactions. Although eosinophilic esophagitis can present with out endoscopic changes, most patients could have one or more of the following endoscopic findings: esophageal strictures; rings; longitudinal mucosal furrows; or white specks that mimic the appearance of candidal esophagitis. The prognosis is confirmed by esophageal mucosal biopsies exhibiting eosinophils (>15 per highpower field). Motility Disorders Esophageal motility problems are a less widespread explanation for dysphagia than are mechanical causes. Dysphagia as a end result of esophageal dysmotility usually ends in difficulty swallowing both solids and liquids. The analysis of esophageal motility issues is incessantly made using esophageal manometry, which assesses motor operate of the higher and decrease esophageal sphincters and the presence or absence of peristalsis of the esophageal physique. Achalasia: characteristic manometric features of achalasia embody an absence of esophageal peristalsis and failure of the lower esophageal sphincter to relax with swallowing. A selective lack of postganglionic inhibitory neurons innervating the graceful muscle of the esophagus is usually seen, and is thought to result in a hypertensive decrease esophageal sphincter that fails to loosen up with swallowing and results in a practical obstruction. Certain illnesses mimic medical, radiologic, and manometric features of achalasia. Spastic motility issues have been termed distal (or diffuse) esophageal spasm and jackhammer esophagus. Patients with these problems usually present with chest ache along with dysphagia Systemic illnesses corresponding to scleroderma can present with dysphagia. Scleroderma causes hypomotility of the esophagus together with a hypotensive decrease esophageal sphincter and aperistalsis. Clinical Features the clinical historical past is extremely important in evaluating the reason for dysphagia. Dysphagia must be distinguished from globus sensation, which refers to the fixed feeling of a lump or tightness within the throat with none demonstrable abnormality in swallowing. Important questions to ask the affected person with dysphagia embrace the time of onset of symptoms, progression, severity, 26 Luminal Gastrointestinal Tract and sample (intermittent or constant) of signs, presence of heartburn, sort of meals that induces signs (liquids or solids, or both), history of head and neck malignancy or surgery, and related neurologic issues. Typical symptoms of oropharyngeal dysphagia embrace choking, cough, or shortness of breath with swallowing. Patients often have problem initiating a swallow, and level to the throat as the placement the place the food is stuck. Other related signs embody dysarthria, nasal speech, hoarseness, weight reduction, and recurrent pulmonary infections. Symptoms of esophageal dysphagia embrace a sensation that food is caught in the chest or throat.
Diseases
After removal of the parotid gland quick allergy treatment 10 mg zyrtec discount free shipping, affected person is having sweating on cheeks while eating allergy medicine making symptoms worse 5 mg zyrtec order overnight delivery. Auriculotemporal nerve which contains parasympathetic secretomotor fibers to parotid gland have reinnervated which nerve Tympanic nerve � Inferior salivatory nucleus sends preganglionic parasympathetic fibres via tympanic department of glossopharyngeal nerve allergy forecast jonesboro ar zyrtec 5 mg buy low price, which forms tympanic plexus in the middle ear cavity, and sends fibres by way of lesser petrosal nerve to attain the otic ganglion. Parasympathetic secretomotor fibres to the parotid gland are carried by the lesser petrosal and never the greater petrosal nerve. Greater petrosal nerve carries secretomotor fibres to the pterygopalatine ganglion and supplies the lacrimal, nasal and palatine glands. Secretory fibres to the parotid gland start within the inferior salivatory nucleus (brainstem) glossopharyngeal nerve tympanic department tympanic plexus lesser petrosal nerve otic ganglion auriculotemporal nerve parotid gland. Tympanic plexus is present in the center ear and receives the preganglionic fibres from the glossopharyngeal nerve. Otic ganglion lies simply inferior to the foramen ovale, via which the lesser petrosal nerve passes and carries the preganglionic fibres to the ganglion. Auriculotemporal nerve is a branch of mandibular nerve, which carries the postganglionic fibres from the otic ganglion to the parotid gland. Buccal � � � � � � � this is a case of post-parotidectomy gustatory sweating, resulting in sweating on the cheek (buccal nerve territory). They can appear when the affected particular person eats, sees, desires, thinks about or talks about certain kinds of food which produce robust salivation. If the sweating was mentioned in the pre-auricular space, the answer would have been nice auricular nerve. The etiology generally is injury to the auriculotemporal nerve which provide sensory fibres to the preauricular and temporal areas, carries parasympathetic fibres to the parotid gland and sympathetic vasoconstrictor and sudomotor fibres to the skin of the identical area. Injury to the auriculotemporal nerve denervates the sweat glands and the vessels of the pores and skin over its distribution, in addition to producing the sensory disturbance. Both the parasympathetic and sympathetic nerves of the face are cholinergic, hence suitable, and within the process of regeneration, parasympathetic fibres turn out to be misdirected and grow along sympathetic pathways. Gustatory sweating is mainly observed within the area of previous parotid lobe elimination, however can be present in other areas deriving their sensory supply from the buccal, higher auricular and lesser occipital nerves. Related to facial nerve � Parotid gland is enclosed in a capsule fashioned by investing layer of deep cervical fascia. Parotid lymph nodes lie partly in the superficial fascia and partly deep to deep fascia over the parotid gland. Pharynx examination is unnecessary � In pathological enlargement of parotid gland, pharynx examination is necessary since, medial border of gland is expounded to the lateral wall of oropharynx (dig). Submandibular and Sublingual Glands Submandibular gland is current within the submandibular triangle lined by the investing layer of the deep cervical fascia. It wraps across the posterior border of mylohyoid, has a big half superficial to the muscle and a small part which lies deep to the muscle. The deep portion is located between the hyoglossus and styloglossus muscular tissues medially and the mylohyoid muscle laterally and between the lingual nerve above and the hypoglossal nerve under. Next it runs between the sublingual gland and the genioglossus and drains on the summit of the sublingual papilla (caruncle) in conjunction with the frenulum of the tongue. They emerge from the brainstem in the nervus intermedius and leave the primary facial nerve trunk in the middle ear to be a part of the chorda tympani, which subsequently joins the lingual nerve. Postganglionic fibres innervate the submandibular, sublingual and lingual salivary glands; some axons re-enter the lingual nerve to entry the lingual glands, while others move directly along blood vessels to enter the submandibular and sublingual glands. Stimulation of the chorda tympani has a direct secretomotor effect and also dilates the arterioles in each the glands. Superior salivatory nucleus sends the parasympathetic preganglionic secretomotor fibres by facial nerve chorda tympani nerve submandibular ganglion. The publish ganglionic fibres are carried by the lingual nerve (branch of mandibular, trigeminal). The facial artery and vein are divided as they course by way of the deep a part of the gland. The post ganglionic fibres are carried by the lingual nerve (branch of mandibular, Trigeminal). Thus, the gland has a large half superficial to the muscle and a small part which lies deep to the muscle. Submandibular duct runs medial to after which superior to the lingual nerve (lingual nerve loop under submandibular duct). Submandibular duct runs anteriorly between the lingual nerve and hypoglossal nerve, that are prone to be injured in dissection within the area. Marginal mandibular department of facial nerve passes posterior inferior to angle of jaw, and is prone to injury in the excision. It is the lingual nerve and not the hypoglossal which loops underneath the submandibular duct. Damage to the lingual nerve causes loss of sensation to the anterior 2/3 of the tongue. The submandibular gland is seen to wrap around the posterior border of mylohyoid Tonsils Tonsils are aggregations of lymphoid tissue located within the posterior wall of the pharynx, which lure bacteria and viruses Waldeyer Tonsillar Ring is collection of lymphoid tissue at the oropharyngeal isthmus, formed by the pharyngeal, palatine, tubal and lingual tonsils encircling the again of the throat (refer). Pharyngeal Tonsil is current within the posterior wall and roof of the nasopharynx and is (called adenoid if enlarged). Tubal (Eustachian) Tonsil is a group of lymphoid nodules near the pharyngeal opening of the auditory tube. Lingual Tonsil is a collection of lymphoid follicles on the posterior portion of the dorsum of the tongue. A triangular fold (plica triangularis) of mucous membrane extends from anterior pillar to the anteroinferior part of tonsil and encloses an area called anterior tonsillar area. Its medial floor is covered by a semilunar mucosal fold (Plica semilunaris), extending between anterior and posterior pillars and enclosing a possible house known as supratonsillar fossa. Lingual artery is a branch of exterior carotid artery which supplies dorsal lingual branches to the tonsil. Ascending palatine artery is a branch of facial artery, which also supplies the tonsil. The upper pole of the tonsil also receives branches from the ascending pharyngeal artery (branch of external carotid artery), which enter the tonsil posteriorly, and from the descending palatine artery (branch of maxillary artery) and its branches, the higher and lesser palatine arteries. Lymphatic drainage (palatine tonsil): Tonsillar lymphatics drain to the higher deep cervical lymph nodes immediately (especially the jugulodigastric nodes) or indirectly via the retropharyngeal lymph nodes. The jugulodigastric nodes are enlarged in tonsillitis, and are palpable superficially 1�2 cm below the angle of the mandible. Adenoids (nasopharyngeal tonsil) is a subepithelial assortment of lymphoid tissue at the junction of roof and posterior wall of nasopharynx. Adenoid are present at delivery, reveals physiological enlargement up to the age of six years after which tends to atrophy at puberty and nearly completely disappears by the age of 20. The arterial provide is by ascending palatine branch of facial, ascending pharyngeal department of external carotid artery, pharyngeal branch of the third a half of maxillary artery, ascending cervical department of inferior thyroid artery of thyrocervical trunk. Lymphatics move to jugulo omohyoid node � � � � � � � � � � Tonsil develops in the area of pharyngeal pouch two, whose endoderm types the tonsillar epithelium. It is present on all sides of the oropharynx in an interval between the palatoglossal and palatopharyngeal folds and primarily provided by facial artery branches. It receives branches of the glossopharyngeal nerve and the lesser palatine department of the maxillary nerve. Since the glossopharyngeal nerve additionally provides ear area, any pathology of the tonsil and tonsillar fossa could additionally be accompanied by pain referred to the ear. Lymphatics drain to the upper deep cervical lymph nodes immediately (especially the jugulodigastric nodes). The higher pole of the tonsil also receives branches from the ascending pharyngeal artery, which enter the tonsil posteriorly, and from the descending palatine artery and its branches, the higher and lesser palatine arteries. Ascending palatine department of facial artery contributes to blood supply of adenoids. Palatine Tonsil is current on both sides of the oropharynx in an interval between the palatoglossal and palatopharyngeal folds. The tonsillar bed is shaped (from inside outwards) by: Pharyngobasilar fascia, superior constrictor muscle and buccopharyngeal fascia. Tonsil is supplied by the branches of the glossopharyngeal nerve and the lesser palatine branch of the maxillary nerve. Glossopharyngeal nerve Palate Palate varieties the roof of the mouth and the ground of the nasal cavity and is of two sorts; Hard and gentle. Hard Palate is the anterior four-fifths of the palate and types a bony framework covered with a mucous membrane between the nasal and oral cavities.

Adequate information of the regional anatomy and morphometric parameters of the vertebrae allergy symptoms beer zyrtec 10 mg, thorough preoperative imaging assessment juniper allergy treatment zyrtec 10 mg sale, respect of anatomical landmarks during screw application allergy forecast richmond va cheap zyrtec 5 mg on-line, and orderly efficiency of all steps of the 31. Once the preliminary trajectory is ready, the boundaries of the trajectory must be carefully inspected utilizing a tactile probe. Although Gertzbein and Robbins considered a mediolateral safe zone of �2 mm surrounding the borders of the pedicle in the thoracic area,59 latest publications have prolonged this security zone up to 2 and 4 mm on the medial and lateral border of the thoracic pedicles, respectively. The surgeon ought to anticipate insufficient bone buy for which solutions need to be available. If a dural tear does happen, a main restore of the tear is preferred, and meticulous watertight closure of the fascia is required. They could additionally be asymptomatic, cause acute symptoms, or lead to late manifestations as part of an erosive process with aneurysm or pseudoaneurysm formation, particularly with regard to pulsatile arterial vessels. The management of asymptomatic sufferers with screws in touch with the vascular buildings recognized postoperatively is commonly unclear. Preparation of the pilot trajectory (drilling or probing) should be limited to barely longer than the pedicle length to avoid violation of anterior vertebral cortex. Major acknowledged surgery-related risk elements are the posterior approach, presence of instrumentation, blood loss especially related to blood transfusion, longer length of surgical procedure, and concomitant autologous bone graft harvest procedure. If the broken screw jeopardizes neurovascular structures, removing with specific instruments, osteotomy, or even an anterior strategy in circumstances of migration might be required. Complex interplay of multiple threat elements together with patient-related, procedure-related, and Kim et al. Second, pediatric deformities commonly contain the thoracic spine with small endosteal pedicle width. A meta-analysis reported the next screw-related complications for neuromuscular scoliosis: revision surgical procedure because of removal or extension 7. Painful root irritation was reported in 2% of the sufferers, whereas neurologic deficit and dural tear occurred in lower than 1%. The spine surgeon must be cognizant of the potential intraoperative and postoperative complications of the screwrelated techniques and have deep familiarity with several different strategies for prevention and administration of those complications. Atlantoaxial fusion with screw-rod constructs: meta-analysis and evaluation of literature. Risk of vertebral artery injury: comparison between C1-C2 transarticular and C2 pedicle screws. The ponticulus posticus: implications for screw insertion into the primary cervical lateral mass. Comparison of security and stability of C-2 pars and pedicle screws for atlantoaxial fusion: meta-analysis and review of the literature. Preoperative radiographic elements and surgeon experience are associated with cortical breach of C2 pedicle screws. Clinical and computed tomographic evaluation of security and efficacy of facet screw fixation in the subaxial cervical spine. Lateral mass screw fixation in the cervical backbone: a systematic literature evaluate. Outcome of 51 circumstances of unilateral locked cervical sides: interspinous braided cable for lateral mass plate fusion compared with interspinous wire and aspect wiring with iliac crest. Screw-related issues in the subaxial cervical spine with the use of lateral mass versus cervical pedicle screws: a systematic review. The location of the vertebral artery foramen and its relation to posterior lateral mass screw fixation. The anatomic relation of lateral mass screws to the spinal nerves: a comparison of the Magerl, Anderson, and An methods. Quantitative anatomic analysis of cervical lateral mass fixation with a comparability of the Roy-Camille and the Magerl screw strategies. Poor surgical technique in cervical plating leading to vertebral artery harm and brain stem infarction -case report. Cervical pedicle screw fixation in one hundred cases of unstable cervical accidents: pedicle axis views obtained utilizing fluoroscopy. Safety and efficacy of pedicle screw placement for grownup spinal deformity with a pedicle-probing conventional anatomic approach. Clinically relevant problems related to pedicle screw placement in thoracolumbar surgical procedure and their administration: a literature review of 35,630 pedicle screws. Spontaneous stomach aortic rupture from erosion by a lumbar backbone fixation system: a case report. The comparability of pedicle screw and cortical screw in posterior lumbar interbody fusion: a potential randomized noninferiority trial. Early medical results with cortically based pedicle screw trajectory for fusion of the degenerative lumbar spine. Pediatric pedicle screws: comparative effectiveness and safety: a systematic literature evaluation from the Scoliosis Research Society and the Pediatric Orthopaedic Society of North America task pressure. Stabilization of the lower thoracic and lumbar spine with exterior skeletal fixation. A biomechanical comparability of supplementary posterior translaminar facet and transfacetopedicular screw fixation after anterior lumbar interbody fusion. Less invasive posterior fixation method following transforaminal lumbar interbody fusion: a biomechanical analysis. Minimally invasive anterior lumbar interbody fusion adopted by percutaneous translaminar side screw fixation in elderly sufferers. A comparison of long-term outcomes of translaminar aspect screw fixation and pedicle screw fixation: a prospective study. A prospective, cohort research comparing translaminar screw fixation with transforaminal lumbar interbody fusion and pedicle screw fixation for fusion of the degenerative lumbar backbone. Interspinous Spacer Complications 32 Interspinous Spacer Complications William Ryan Spiker and Alan S. Diagnosis requires both medical symptoms and evidence of narrowing of the lumbar spinal canal on imaging studies. Surgery is carried out with the objective of reducing positional buttock and leg pain (neurogenic claudication) however may not scale back again ache due to degenerative illness. Interspinous spacers are a less-invasive surgical remedy choice for sufferers with intermittent neurogenic claudication attributable to spinal stenosis. Interspinous spacers are positioned between the spinous processes on the stage of stenosis to restrict extension and supply interlaminar stabilization. This local kyphosis/flexion enlarges the spinal canal at that degree and mimics the symptomatic relief of flexion in this patient population. Interspinous spacers are placed through a posterior incision with the patient in a inclined or lateral decubitus place. After pores and skin incision, the supraspinous and interspinous ligaments are uncovered; for some gadgets, such because the X-Stop, the supraspinous and interspinous ligaments are preserved. The units are then secured to the spinous process(es), limiting local extension by resisting compression of the posterior parts. The capacity of the spacer to resist compression is dependent on the bone high quality of the spinous course of. Interspinous spacers are typically not accredited to be used in instances with important instability (fracture or unstable spondylolisthesis), deformity (scoliosis > 25 degrees), ankylosis or previous fusion of the affected level, extreme osteoporosis, stenosis at greater than two ranges, or cauda equina syndrome. Proposed indications for these devices embody therapy of lumbar spinal stenosis in sufferers with grade I degenerative spondylolisthesis, mild scoliosis, discogenic low again ache, recurrent lumbar disc herniation, and aspect syndrome. Adverse occasions frequent to all posterior lumbar spine surgery embody the following: wound infections, medical complications (blood clots, heart attack, stroke), want for blood transfusion, neurologic damage, need for revision surgical procedure, and worsening of leg and again symptoms. Interspinous Spacer Complications Because spacer placement can be performed through a small incision with minimal soft tissue dissection and relatively brief operative instances, some complications (such as wound infections and blood clots) may be less frequent with spacer placement than with basic open decompression methods. Unique complications associated with interspinous spacer insertion include spinous process fracture and gadget dislocation. Strict inclusion criteria were used for the research, including age > 50 years, intermittent neurogenic claudication resolved by sitting, radiographic spinal stenosis, and failure of 6 months of nonoperative therapy. At 2-year follow-up, they discovered that the operatively treated patients had superior outcomes to the nonoperatively handled sufferers that had been statistically significant. In one other prospective randomized trial, Anderson et al10 evaluated the X-Stop in patients with grade I degenerative spondylolisthesis and spinal stenosis. With an understanding that interspinous spacers are probably more practical than nonoperative modalities for sufferers with neurogenic claudication, a current potential, randomized managed trial compared the Coflex interspinous spacer with the "present normal of care"-a posterior decompression and instrumented fusion. In total, 322 sufferers had been included within the examine and 96% of members completed 2-year follow-up. Patient satisfaction scores and radiographic preservation of adjacent degree biomechanics had been both found to be statistically superior to fusion.
Laboratory exams allergy nose sprays cheap 10 mg zyrtec amex, including a complete blood depend and comprehensive metabolic panel allergy forecast montreal quebec best 5 mg zyrtec, are regular aside from a mildly elevated serum alkaline phosphatase stage allergy symptoms morning and night zyrtec 10 mg buy discount on-line. Laboratory exams show a white blood cell depend of 24 000 mm�3 with 89% neutrophils, serum aspartate aminotransferase stage a hundred twenty five U l�1, alanine aminotransferase 214 U l�1, and bilirubin 5 mg dl�1. Right higher quadrant ultrasonography shows cholelithiasis, with no evidence of cholecystitis, and a dilated bile duct with intraductal stones. Laboratory checks present a white blood cell rely of 18 000 mm�3, serum alkaline phosphatase degree four hundred U l�1, aspartate aminotransferase 200 U l�1, alanine aminotransferase 216 U l�1, and bilirubin 4 mg dl�1. He continues to be febrile despite treatment with broadspectrum antibiotics for twenty-four hours. Laboratory tests present a white blood cell depend of 27 000 mm�3 and elevated serum alkaline phosphatase and bilirubin ranges. Ultrasonography shows gallbladder wall thickening, and air in the 336 Pancreas and Biliary System gallbladder wall. Ultrasonography shows proof of gallstones however no other abnormality; the liver dimension is normal. Laboratory checks including serum aminotransferase, alkaline phosphatase, and bilirubin ranges are regular. Answers 1 A the patient describes signs according to biliary pain, doubtless from cholelithiasis. The differential prognosis includes choledocholithiasis, cholecystitis, pancreatitis, gastroesophageal reflux disease, and peptic ulcer illness. Acute cholangitis is attributable to a stone impacted within the bile duct, with secondary bacterial proliferation. It is in all probability going that this affected person has black pigment stones, given his historical past of sickle cell illness. Irrespective of the sort of gallstone, the treatment of alternative for acute cholangitis is broadspectrum antibiotics adopted by biliary decompression. B the affected person has acute cholangitis as evidenced by fever, belly ache, jaundice, and altered mental standing. Cholangitis is a lifethreatening situation and requires urgent biliary decompression. If the patient is hemodynamically unstable, percutaneous cholecystostomy should be carried out. C Air within the gallbladder wall is indicative of emphysematous cholecystitis, which has a high mortality and morbidity � hence the necessity for urgent remedy. Antibiotic protection should be initiated and adopted immediately by a cholecystectomy. Stones in the bile duct, even when asymptomatic, should be eliminated due to an elevated risk of complications. The risk of gallbladder malignancy is markedly elevated in Native Americans with gallstones; due to this fact, in this case, as properly as in sufferers with calcifications in the gallbladder wall (porcelain gallbladder), cholecystectomy is indicated. He was working at his laptop, started to really feel nauseated, and vomited two cups of brilliant pink blood. Vital indicators show a blood strain of 145/86 mmHg supine and 100/65 mmHg upright; pulse price 112 per minute supine and one hundred thirty per minute upright; respiratory rate 14 per minute; and oxygen saturation 94% on room air. Laboratory exams show a white blood cell count of 7200 mm�3, hemoglobin stage 10 g dl�1, platelet count one hundred 000 mm�3, and mean corpuscular volume ninety nine fl. Melena is black, tarry, malodorous stool that often signifies hemorrhage proximal to the ligament of Treitz. Occasionally, bleeding from a source in the small bowel or right colon can also cause melena. The black color is attributable to oxidation of the iron in hemoglobin by gastric acid or by bacteria. Less widespread causes of peptic ulcer include Cushing ulcer (gastric and duodenal ulcers associated with elevated intracranial pressure) and Curling ulcer (acute ulcer of the duodenum related to severe burns). Common causes of erosive esophagitis in immunocompetent patients embrace gastroesophageal reflux illness and radiation therapy. In immunosuppressed persons, erosive esophagitis is usually attributable to infections, similar to Candida spp. Hemosuccus pancreaticus (bleeding into the pancreatic duct) might happen with acute or continual pancreatitis, pancreatic most cancers, or pancreatic duct manipulation. Aortoenteric fistula (communication between the stomach aorta, usually an aneurysm or graft, and the third portion of the duodenum). They are extra common in persons >65 years of age and in these with chronic constipation. Angiodysplasias (or angioectasias) are ecstatic thinwalled venules or capillaries in the mucosa or submucosa. They may also bleed within the setting of uremia because of platelet dysfunction from uremia. Most current as chronic occult blood loss and irondeficiency anemia quite than acute blood loss. Causes of colitis embody ischemia, an infection, radiation therapy, and inflammatory bowel disease. Bleeding from internal hemorrhoids is typically intermittent, small in quantity, and selflimited however could be massive, leading to hemodynamic compromise. Clinical Features History the onset, duration, severity, and character of emesis (bright purple blood, espresso ground), amount of emesis, and presence of melena or hematochezia and related nausea, retching, and abdominal pain must be determined. Associated signs including longstanding heartburn, continual constipation, diarrhea, and nosebleeds ought to be ascertained. The historical past must also embrace an evaluation of risk factors for liver disease corresponding to a history of illicit drug use, alcohol abuse, blood transfusions and unprotected sex, as properly as a household history of liver disease. Gingko biloba (a natural supplement) and selective serotonin reuptake inhibitors may improve the chance of bleeding. The family history ought to embrace liver illness, bleeding problems, cancer, and inflammatory bowel disease. Patients ought to be evaluated instantly for symptoms and indicators of shock, and people with out overt tachycardia or hypotension must be examined for orthostatic hemodynamic adjustments. An improve within the pulse price of 20 per minute and a drop in blood stress of 20 mmHg systolic or 10 mmHg Acute Gastrointestinal Bleeding 349 diastolic from the supine to standing position point out roughly 700 ml of blood loss. Lightheadedness or dizziness when standing from a sitting position is a sensitive marker for the presence of orthostasis. Peritoneal signs (abdominal rebound tenderness, guarding, or rigidity) might indicate a perforated ulcer, perforated colon (from ischemic colitis, inflammatory bowel disease), or poisonous megacolon (due to inflammatory bowel disease). Hemodynamic instability or proof of great ongoing blood loss (active hematemesis, melena, or at least reasonably extreme hematochezia) is a sign for admission to an intensive care unit for shut monitoring. Intubation may be required for protection of the airway in sufferers with large hematemesis. Laboratory checks together with a complete blood rely, complete metabolic panel, prothrombin time, and partial prothrombin time ought to be obtained in all sufferers. Antibiotics scale back the incidence of spontaneous bacterial peritonitis associated with acute variceal bleeding. Insertion of a Sengstaken�Blakemore or Minnesota tube could additionally be necessary for enormous variceal hemorrhage. These tubes have gastric and esophageal balloons that might be inflated to tamponade varices. A bleeding (tagged purple blood cell) scan makes use of technetium sulfur colloid labeled autologous purple blood cells, that are infused back into the patient to detect the positioning of bleeding. In sufferers who proceed to bleed and are hemodynamically unstable, multidetector computed tomography angiography may be diagnostic, and angiography may be diagnostic and therapeutic (with embolization or intra arterial infusion of vasopressin). Surgery may be required for uncontrolled bleeding or in some instances of recurrent diverticular bleeding, which may occur in as a lot as 35% of instances. Bleeding from esophageal or gastric varices carries a mortality rate of 50% if untreated. A 27yearold man presents to the emergency division with three episodes of brilliant red blood per rectum the day after completing a marathon. His very important signs include a blood stress of 95/50 mmHg and pulse rate 112 per minute.
Lysine Monohydrochloride (Lysine). Zyrtec.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96265
Bridging necrosis and cirrhosis are just like allergy medicine everyday buy zyrtec 10 mg overnight delivery that seen in other continual liver diseases allergy medicine like singular zyrtec 5 mg purchase with visa. Primary Sclerosing Cholangitis Primary sclerosing cholangitis is a cholestatic liver illness characterized by inflammation of both intrahepatic and extrahepatic bile ducts allergy forecast kansas city zyrtec 5 mg purchase overnight delivery, resulting in multi focal bile duct strictures. Small duct primary sclerosing cholangitis is a variant with characteristic histologic features but normal cholangiography. Microscopic Features Early in the illness process histologic findings are sometimes nonspecific. Primary sclerosing cholangitis is histologically characterised by progressive periductal fibrosis. It is seen most frequently in individuals with features of metabolic syndrome, and is a severe type of nonalcoholic fatty liver illness. Hepatocyte ballooning is characterized by loss of regular hepatocyte shape, with swelling and enlargement of the hepatocytes. These are neoplasms of the pancreatic ductal system that are characterised by dilated main pancreatic duct or facet branches. Note the papillary epithelial lining with hyperchromatic nuclei, loss of polarization, and outstanding nucleoli. Microscopic Features Typical findings on cytology include mucinous columnar cells that stain optimistic for mucin. Mucinous Cystic Neoplasm of the Pancreas Mucinous cystic neoplasms are a subtype of pancreatic cystic neoplasm which are nearly exclusively seen in females and often current as an incidental find ing on imaging. These have a moderate malignant potential and are handled with surgical resection. Classic Pathology 469 Microscopic Features Typical cytology findings embody columnar cells that stain constructive for mucin. Serous Cystic Tumors of the Pancreas Serous cystic tumors are a subtype of pancreatic cystic neoplasms. They are mostly seen in older girls in the fifth to seventh decade of life. Solid Pseudopapillary Tumors of the Pancreas Solid pseudopapillary tumors are a uncommon subtype of pancreatic cystic neoplasms. They have average to excessive malignant potential and are treated with surgical resection. Microscopic Features Typical cytology contains branching papillae with myxoid stroma. Photomicrograph displaying a highpower view of a serous cystadenoma with variably sized cysts lined by compressed tumor cells and extra stable areas comprised of bland tumor cells with spherical nuclei and clear cytoplasm. It is a mature assortment of fluid around the pancreas that sometimes develops as a complication of pancreatitis. Microscopic Features Typical cytologic features embrace the presence of neutrophils, macrophages, and histiocytes with adverse staining for mucin. Anterior Cranial Fossa, Nasal Cavity, and Paranasal Sinuses 1 Anterior Cranial Fossa, Nasal Cavity, and Paranasal Sinuses Sheldon D. Understanding the shut relationship, patterns of illness unfold, and potential issues is crucial for optimum diagnostic analysis of this space. In the case of malignant illness, correct identification of tumor extent is essential for acceptable staging and preoperative planning and to guarantee an optimum resection margin and the best possible consequence for the affected person. In order to help higher perceive the anatomic pathways of illness unfold and anatomic variants that may predispose to issues and are of significance for surgical planning, this chapter will start with a quick overview of embryologic growth, followed by a clinically oriented evaluation of imaging anatomy. The orbitosphenoid cartilage, alisphenoid cartilage middle, and condensed mesenchyme (intramembranous bone) give rise to the extra lateral parts of the sphenoid/sphenoid wings. However, small gaps might persist in the nasal roof until 3 years of age and the foramen cecum may ossify as late as 5 years of age. From the fifth week of gestation, the nasal pits deepen toward the oral cavity, ultimately leading to an open communication between the oral and nasal cavities. An elaborate cascade of development and fusion then results in the downward progress of the nasal septum, formation of the definitive secondary palate, and other buildings constituting the nasal cavity. Ectodermal epithelium on the roof of the nasal cavity differentiates into the olfactory epithelium, with the development of olfactory receptor cells having axons that lead into the growing olfactory bulbs. All paranasal sinuses begin as evaginations or diverticula situated along the walls of the nasal cavities that evolve into airfilled cavities in the adjacent bones. Full improvement of the maxillary sinuses occurs after eruption of permanent maxillary dentition at approximately 20 years of age. A detailed discussion of the embryological growth of the anterior cranium base and paranasal sinuses is beyond the scope of this chapter and lined intimately elsewhere. The skull base is shaped mainly by endochondral ossification, whereas the calvarial vault is mainly shaped by membranous ossification. Occasionally, the frontal sinus may develop from an ethmoid air cell that has migrated from the ethmoid infundibulum rather than the frontal recess. The main development of the frontal sinus occurs in the postnatal period, with the sinus slowly enlarging to attain maximal adult dimension close to the top of the second decade of life. Conversion of pink to fatty marrow happens between 7 and 24 months of age and is believed to first begin in the presphenoid. The sphenoid sinus starts its main development in the third to fifth yr of life, typically reaching grownup configuration by the age of 12 years. In rare cases, untimely arrest of sinus development is proposed as a possible etiology for alterations in the appearance of the cranium base that may mimic pathology, referred to as arrested pneumatization of the cranium base. The anterior skull base could be broadly described as constituting the ground of the anterior cranial fossa, roof of the nostril, ethmoid air cells, and orbits anteriorly and the lesser wings and anterior physique of the sphenoid bone (planum sphenoidale) posteriorly. Cribriform plate/ethmoid bone (purple), frontal bones (tan), occipital bone (green), parietal bones (pink), sphenoid bone (red), temporal bones (grey). Illustration of the extracranial facet of the cranium base, with the orbital roofs, ethmoid air cells, and sphenoid sinus exposed. The anterior cranium base can be broadly described as constituting the floor of the anterior cranial fossa, roof of the nose, ethmoid air cells, and orbits anteriorly and the lesser wings and anterior physique of the sphenoid bone posteriorly. The anterior clinoid processes are formed by the medial a part of the lesser wings of the sphenoid and serve as websites of attachment for the anterior part of the tentorium cerebelli anteriorly. The anterolateral boundary of the anterior skull base is formed by the frontal bones. Other bony landmarks of the anterior cranium base include the frontal crest and crista galli. Although pneumatization of this structure represents an anatomic variant, there could be inflammation of the pneumatized crista galli just like paranasal sinuses and there are even case reviews of mucocele formation on this area. The cribriform plate incorporates multiple small perforations that transmit afferent fibers from the nasal mucosa to the olfactory bulbs. At the junction of the ethmoid (cribriform plate) and the adjacent frontal bone, the frontoethmoidal suture incorporates the foramen cecum, similar to a small midline pit anterior to the crista galli. The data on the event, patency, and presence of a practical vein through the foramen cecum is sparse. However, though absent in the majority of the inhabitants, there may be rare cases of a patent small emissary vein in children and rarely in adults that interconnects the venous system of the nasal cavity and the superior sagittal sinus. Similarly, the posterior ethmoidal canals and attendant neurovascular contents are transmitted by way of the skull base on the junction of the posterolateral corners of the cribriform plate and the sphenoid. The anterior skull base has important relations to crucial adjacent constructions and areas that have to be taken into account when evaluating totally different pathology in addition to for therapy planning. Superiorly, these are the buildings of the anterior cranial fossa, together with the frontal lobes as properly as the olfactory bulb and tract (olfactory nerve or cranial nerve 1). Inferiorly, these are the nasal cavity and ethmoid air cells medially and the orbits laterally. The applied anatomy of the nasal cavity and paranasal sinuses will be discussed in the next part. Posteriorly, the nasal cavity roof is shaped by the anterior aspect of the body of the sphenoid and the superior turbinates, with bilateral interruptions for the sphenoid sinus ostia. Anteriorly, the nasal cavity roof slopes down alongside the inner side of the nasal bones and nasal spine of the frontal bone. The olfactory fossa is fashioned by the cribriform plate, separated at the midline by the crista galli. In a classic examine in 1962, Keros classified the depth of the olfactory fossa, as defined by the height of the lateral lamina of the cribriform plate, into three classes.
Fluid collections brought on by inflammatory processes are often a lot thicker as a result of they contain pus allergy medicine eye drops buy zyrtec 10 mg free shipping, fibrin or blood allergy medicine high purchase 10 mg zyrtec free shipping. These elements predispose to the formation of localized fluid collections allergy testing baltimore zyrtec 5 mg buy discount, which can turn out to be walled-off because the inflammatory process progresses. These methods supply reliable and versatile methods of accessing peritoneal areas, together with comparatively inaccessible subhepatic, perihepatic or intermesenteric collections. A posteriorly perforating ulcer in the pyloric antrum of the abdomen is more likely to produce preliminary localized peritonitis or abscess formation within the: a. Which of the next peritoneal recesses is continually current in infants but disappears with age: (Delhi 06) a. In which of the next vessels transverse mesocolon seen: (All India Dec 13 Pattern) a. Left subhepatic � Left subhepatic house is the other name for the lesser sac (omental bursa). Hepatic vein � Right tree margin of lesser omentum incorporates:- (i) Hepatic artery proper, (ii) Portal vein, (iii) Bile duct,(iv) Lymph nodes and lymphatics,and (v) Hepatic plexus of nerves. Anterior wall:- Caudate lobe of liver,abdomen,lesser omentum,and 2nd layer of higher omentum. Posterior wall:- third layer of greater omentum, and structures forming abdomen mattress (transverse colon, transverse mesocolon, diaphragm,left kidney,left suprarenal gland, pancreas and splenic vessels). Right border:- Right free margin of larger omentum and floor of epiploic foramen four. Left border:- Left free margin of greater omentum;gastrosplenic, linorenal and gastrophrenic ligaments. Omental bursa � A posterior gastric ulcer might perforate into the lesser sac (omental bursa). Inferior liver � Epiploic foramen (foramen of winslow or aditus to lesser sac) is a slit like opening by way of which lesser sac communicates with higher sac. Its boundaries are:� Anterior:- Right free margin of lesser omentum (contains portal vein,hepatic artery correct and bile duct). Left subhepatic house � Lesser sac (Omental bursa) is left posterior intraperitoneal house, also known as left subhepatic house. Uterus and rectum � In females rectouterine pouch (pouch of Douglas) lies between rectum (posteriorly) and uterus and posterior fornix of vagina (anteriorly). Inferior mesenteric vein � Inferior mesenteric vein lies in the free fringe of the peritoneal fold of paraduodenal recess. Intersigmoid recess � Intersigmoid recess is constantly present in the foetus and in early infancy, but might disappear with age. Left ureter � Left ureter crossing the bifurcation of left frequent iliac artery lies behind intersigned recess, which is a surgical information for locating left ureter. Middle colic artery Mesentery of intestine Mesentery correct (Mesentery of small intestine) Transverse mesocolon Mesoappendix Sigmoid mesocolon Vessels contained by mesentery Jejunal and ileal branches of superior mesenteric vessels Middle colic vessel Appendicular vessels Sigmoid vessels 15. Fascia between the rectal ampulla and the prostate and the seminal vesicles � Posterior surface of prostate is separated from rectum by the fascia of Denonvilliers which is the obliterated rectovesical pouch of peritoneum. Right and left gastric arteries which provide the lesser curvature (abdominal aorta celiac trunk widespread hepatic Right and left gastroepiploic arteries which provide the greater curvature (abdominal aorta celiac trunk common artery right gastric artery; stomach aorta celiac trunk left gastric artery). Short gastric arteries which provide the fundus (abdominal aorta celiac trunk splenic artery brief gastric arteries). Right and left gastric veins (right and left gastric veins portal vein hepatic sinusoids central veins hepatic veins Left gastroepiploic vein and short gastric veins (left gastroepiploic vein and brief gastric veins splenic vein portal Right gastroepiploic vein (right gastroepiploic vein superior mesenteric vein portal vein hepatic sinusoids central veins hepatic veins inferior vena cava). Innervation the innervation of the stomach is by the enteric nervous system which in the stomach consists of the myenteric plexus of Parasympathetic Preganglionic neuronal cell bodies are situated in the dorsal nucleus of the vagus. The enteric nervous system is modulated by the parasympathetic and sympathetic nervous techniques. Sympathetic Preganglionic neuronal cell our bodies are situated within the intermediolateral cell column of the spinal twine (T5 to T9). Postganglionic axons synapse in the complicated circuitry of the enteric nervous system. Gastric ulcers most frequently happen inside the physique of the abdomen along the lesser curvature above the incisura angularis. Carcinomas of the abdomen are mostly found within the pylorus of the stomach and may metastasize to supraclavicular lymph nodes (Virchow nodes) on the left side which may be palpated inside the posterior triangle of the neck. The short gastric arteries, left gastroepiploic artery and, when present, the posterior gastric artery are branches of the splenic artery. The proper gastric artery and right gastroepiploic artery come up from the hepatic artery and its gastroduodenal branch, respectively. Stomach � Main gastric nerve of Latarjet is department of vagus and supplies the abdomen. All of the above � Arterial provide of stomach is as follows � Along lesser curvature: Left gastric artery (branch of coeliac trunk) and proper gastric artery (branch of correct hepatic artery). Left gastric artery � he constantly largest artery to the stomach is left gastric artery. These structures forming stomach mattress are (i) Diaphragm,(ii) left kidney, (iii) left suprarenal (adrenal) gland, (iv) pancreas (body), (v) transverse colon, (vi) splenic flexure of colon and (vii) splenic artery. Pre aortic nodes Lymphatic drainage of stomach � the abdomen can be divided into four lymphatic territories. Lymph vessels from these nodes journey alongside the splenic artery to reach the coeliac nodes. Lymph vessels arising in these nodes drain into the first and second elements of the duodenum. From right here the lymph is drained further into the hepatic nodes that lie along the hepatic artery; and finally into the coeliac nodes. From here it passes through the intestinal lymph trunk to attain the cisterna chyli. Superior Part (First Part) the primary 2 cm of the superior part is intraperitoneal and therefore has a mesentery and is cell; the remaining distal three cm of the superior part is retroperitoneal. Radiologists check with the primary 2 cm of the superior a part of the duodenum because the duodenal cap or bulb. The superior half begins at the pylorus of the stomach (gastroduodenal junction) which is marked by the prepyloric vein. The hepatoduodenal ligament attaches superiorly and the greater omentum attaches inferiorly. Descending Part (Second Part) the descending part is retroperitoneal and receives the widespread bile duct and major pancreatic duct on its posterior/ medial wall at the hepatopancreatic ampulla (ampulla of Vater). In extreme stomach accidents, this part of the duodenum may be crushed towards the L3 vertebra. Ascending Part (Fourth Part) the ascending half is intraperitoneal and ascends to meet the jejunum on the duodenojejunal junction which occurs approximately at the L2 vertebral degree about 2 to 3 cm to the left of the midline. This junction normally types an acute angle which is recognized as the duodenojejunal flexure which is supported by the ligament of Treitz (represents the cranial end of the dorsal mesentery). The arterial provide of the duodenum is from the next: Supraduodenal artery which supplies the upper portion of the duodenum (abdominal aorta celiac trunk common hepatic artery gastroduodenal artery supraduodenal artery). Anterior and posterior superior pancreaticoduodenal arteries (abdominal aorta celiac trunk common hepatic artery gastroduodenal artery anterior and posterior superior pancreaticoduodenal arteries). Anterior and posterior inferior pancreaticoduodenal arteries (abdominal aorta superior mesenteric artery anterior and posterior inferior pancreaticoduodenal arteries). The venous drainage of the duodenum is to the next: Anterior and posterior superior pancreaticoduodenal veins (anterior and posterior superior pancreaticoduodenal veins portal vein hepatic sinusoids central veins hepatic veins inferior vena cava). Anterior and posterior inferior pancreaticoduodenal veins (anterior and posterior inferior pancreaticoduodenal veins superior mesenteric vein portal vein hepatic sinusoids central veins hepatic veins inferior vena cava). Clinical Considerations Duodenal ulcers most frequently occur on the anterior wall of the first part of the duodenum. Perforations of the duodenum occur most often with ulcers on the anterior wall of the duodenum. However, posterior wall perforations may erode the gastroduodenal artery causing severe hemorrhage and lengthen into the pancreas. Different arteries of the duodenum derived immediately or not directly from the above two arteries are: 1. Superior pancreaticoduodenal artery, a department of gastroduodenal artery (a branch of hepatic artery from the coeliac trunk). Respective branches of superior and inferior pancreaticoduodenal arteries anastomose to form anterior and posterior pancreaticoduodenal arterial arcades.
The finest diagnostic test to set up the prognosis of achalasia is which of the following A 65yearold man with intermittent dysphagia is noted to have an esophageal ring on upper endoscopy allergy symptoms due to weather zyrtec 5 mg cheap. A 21yearold man is seen within the clinic for the analysis of painful swallowing and dysphagia for the past 2 weeks allergy relief for dogs purchase 5 mg zyrtec with mastercard. His medications include a steroid inhaler for asthma and doxycycline to treat reasonably extreme acne allergy medicine zyrtec coupons zyrtec 10 mg mastercard. He has occasional heartburn (less than twice per month) and takes ranitidine as needed. In the setting of a prior longterm history of heartburn, the differential analysis contains reflux esophagitis, peptic stricture, or adenocarcinoma of the esophagus. B In achalasia, the postganglionic nitric oxidecontaining neurons are lost, thereby leading to failure of leisure of the lower esophageal sphincter. His symptoms are additionally in keeping with a benign stricture, given his longstanding reflux signs. This presentation could be secondary to stroke, significantly in gentle of the weak spot on his left facet. Esophageal cancer is usually related to weight reduction and progressive dysphagia for strong meals. When esophageal dysphagia is suspected, one should perform a barium esophagogram with or without an upper endoscopy. In a affected person in whom gastroesophageal reflux is a suspected reason for dysphagia, pH testing could additionally be performed. B Achalasia is a motility dysfunction characterised by loss of myenteric ganglion inhibitory neurons resulting in a loss of relaxation of the decrease esophageal sphincter. A videoradiographic study is beneficial for the evaluation of oropharyngeal dysphagia. Upper endoscopy is useful for the detection of a structural lesion causing dysphagia. Esophageal pH testing may help in establishing the function of gastroesophageal reflux as a reason for dysphagia. A the best remedy option for an esophageal ring is to perform an endoscopic dilation. Other medications that may result in pillinduced esophagitis embody aspirin, nonsteroidal antiinflammatory medication, potassium and iron supplements, and bisphosphonates. Although erosive esophagitis is a chance, this affected person has infrequent reflux symptoms, and erosive esophagitis is a much less doubtless cause than pillinduced esophagitis. She describes the discomfort as a continuing uninteresting ache that usually happens postprandially and is related to nausea, however not vomiting. At age forty, she had a colonoscopy for rectal bleeding, which was unremarkable aside from hemorrhoids. Her past medical and surgical history is unremarkable aside from seasonal allergy symptoms. She takes antihistamines for seasonal allergic reactions and ibuprofen 1�2 tablets several occasions a month for complications. Physical examination reveals a blood pressure of 114/80 mmHg, pulse rate 67 per minute, and body mass index 22. The remainder of the examination, including an belly examination, is unremarkable. Helicobacter pylori: � Some 70% of gastric ulcers and 80�95% of duodenal ulcers are attributed to H. The bacterium produces urease, which breaks down urea to ammonia and carbon dioxide and is required for the survival of H. Peptic Ulcer Disease 37 � Lesscommon causes: gastrin hypersecretory states such as gastrinoma (Zollinger�Ellison syndrome), mastocytosis, antral G cell hyperplasia. Clinical Features Typical signs: these happen in <20% of sufferers and embody dyspepsia (epigastric ache, fullness, or bloating, typically with nausea and eructation). With duodenal ulcer, the discomfort typically occurs 1�3 hours after a meal and is relieved by meals or antacids. When present, findings embrace epigastric tenderness and occult blood within the stool, or melena (black or maroon stools ensuing from gastrointestinal bleeding). Peritoneal signs (rebound abdominal tenderness, guarding, and rigidity) signify a perforated ulcer, and a succussion splash is seen with partial or complete gastric outlet obstruction. The benefits and drawbacks of every test should also be considered (Table three. Rapid urease test* Excellent sensitivity and specificity Expensive and requires infrastructure and educated personnel Inexpensive and offers rapid Sensitivity considerably reduced in the posttreatment setting outcomes. Excellent specificity and excellent sensitivity in properly chosen sufferers Excellent specificity. Allows dedication of antibiotic sensitivities Excellent sensitivity and specificity. Allows dedication of antibiotic sensitivities Expensive, difficult to perform, and never broadly out there. Only marginal sensitivity Methodology not standardized across laboratories and never broadly out there 3. Unpleasantness associated with amassing stool * the sensitivity of all invasive and noninvasive exams that identify energetic H. The absence of continual gastritis (inflammation) on histologic examination of a gastric mucosal biopsy specimen is nice proof of the absence of H. Peptic Ulcer Disease 41 Serum Gastrin Level Usually measured if gastrinoma (Zollinger�Ellison syndrome) is suspected (on the premise of recurrent peptic ulcer, severe and multiple ulcers, and concomitant diarrhea). If the level is elevated however <1000 pg ml�1, gastric pH measurement could additionally be performed (pH measurement is finished on gastric fluid obtained via endoscopy or insertion of a nasogastric tube). A secretin stimulation take a look at will verify gastrinoma if the rise in serum gastrin after intravenous administration of secretin is >200 pg ml�1. Treatment Antisecretory agents: administered orally (8 weeks for duodenal ulcer and 8�12 weeks for gastric ulcer). Either triple remedy, a fourdrug concomitant quadruple therapy, or a bismuth quadruple therapy routine is really helpful. Others embody perforation or penetration into the pancreas (5�7%) and gastric outlet obstruction (<5%). Gastroesophageal reflux disease might enhance in frequency or severity after the eradication of H. Pearls Because a small percentage of gastric ulcers are actually ulcerated gastric carcinomas, all gastric ulcers have to be assessed carefully to distinguish a benign from a malignant ulcer. A 30yearold man presents to the emergency department with the sudden onset of severe stomach ache. He states that he has been coaching for a marathon and has been taking ibuprofen for myalgias. D Any of the tests listed can detect signs of a perforated ulcer (free air in the abdomen). Lopez and Edward Lin Clinical Vignette A 64yearold man with a forty packyear smoking history presents with a grievance of severe dysphagia for solids and worsening dysphagia for liquids. The transhiatal method involves an upper midline incision to create a gastric conduit and a left transverse supraclavicular or left neck incision parallel to the sternocleidomastoid to entry and dissect the cervical esophagus. The gastric conduit is then delivered into the posterior mediastinum to create the esophagogastric anastomosis within the cervical area. The Ivor Lewis strategy entails an upper midline incision to create a gastric conduit in a way much like that for the transhiatal strategy, followed by a right thoracotomy to mobilize the intrathoracic esophagus for an intrathoracic anastomosis. The threehole, or McKeown, method is carried out by way of separate higher midline, thoracic, and cervical incisions. This approach is assumed to provide a better exposure to the encircling constructions and to lower the chance of idiopathic harm; it also permits an extensive lymphadenectomy to be performed. Laparoscopic, thoracoscopic, and robotassisted approaches have additionally been employed in the hope of lowering the morbidity of multiple incisions while replicating the results of the open approaches. A feeding jejunostomy may also be positioned for adequate nutritional support during recovery. Indications Malignant neoplasms of the esophagus, together with squamous cell carcinoma, adenocarcinoma, small cell carcinoma, leiomyosarcoma, rhabdomyosarcoma, fibrosarcoma, liposarcoma, lymphomas, and metastatic lesions. Rarely, neuromotor dysfunction of the esophagus similar to achalasia, distal esophageal spasm, or scleroderma. Complications Early postoperative issues of an esophagectomy can involve bleeding as a result of inadequate hemostasis through the operation, arrhythmias, and respiratory issues corresponding to atelectasis and pneumonia.

Minimize duration allergy medicine zyrtec d 5 mg zyrtec discount visa, drive allergy shots and birth control generic zyrtec 5 mg, and frequency of retraction of nerve roots and thecal sac allergy medicine makes me feel high cheap zyrtec 10 mg online. The timing of onset of symptoms is often a key component to prognosis of neurologic problems if no intraoperative issues are noted. Assessment of compressive pathologies including pedicle screws, cages, bone graft, or hematoma/ seromas is necessary to recognize and manage, and ruling out these distinct causes of compression is vital previous to arriving at different diagnoses of exclusion. Failure of surgical success because of neurological compression often requires direct management with revision decompression, no matter timing of onset of signs. Medications mentioned by multiple authors embrace oral corticosteroids or neuropathic agents similar to gabapentin or pregabalin. Often a final resort involves postoperative nerve root blocks or corticosteroid injections if confident that the postoperative symptoms are actually transient as failure of those injections is commonly one of many authentic indications for the surgical procedure. Modifiable affected person elements can embrace patient selection, preoperative decolonization of nares, medical and dietary optimization, and management of immune-modulating, blood glucose, and anticoagulation medicines, as well as threat components for thrombophilia. Prophylactic intraoperative powdered vancomycin applied to the wound previous to closure has been proposed as one method of stopping or lowering postoperative backbone an infection. Furthermore, no cost evaluation was mentioned in relation to the overall value of such a protocol. Despite the revision with autograft interbody help, complete collapse of the disc space occurred with a mean lack of each top (12. Better prevention protocols, earlier diagnostic capabilities, and less morbid remedy strategies are wanted. Intraoperative native vancomycin powder within the wound and/or bone graft could lower an infection rates. Successful therapy is possible with each explantation and retention of the interbody device at time of surgical debridement. Complications of Posterior and Transforaminal Lumbar Interbody Fusion of infectious L3�L4 spondylodiscitis occurred with resultant migration to the left pulmonary artery. Bone union price with autologous iliac bone versus native bone graft in posterior lumbar interbody fusion. Guideline replace for the efficiency of fusion procedures for degenerative disease of the lumbar spine. These techniques permit circumferential lumbar fusion without accessing anterior approaches to the backbone and have developed over time, lowering many of the complications which initially restricted their acceptance. Despite being a helpful and customarily secure process, quite a few potential problems exist and symbolize real challenges to both surgeon and affected person. Clinical course and significance of the clear zone around the pedicle screws within the lumbar degenerative disease. Does the formation of vertebral endplate cysts predict nonunion after lumbar interbody fusion Follow-up of patients with delayed union after posterior fusion with pedicle screw fixation. Prospective medical outcomes of revision fusion surgery in patients with pseudarthrosis after posterior lumbar interbody fusions utilizing stand-alone metallic cages. Heterotopic ossification after transforaminal lumbar interbody fusion without bone morphogenetic protein use. Symptomatic ectopic bone formation after off-label use of recombinant human bone morphogenetic protein-2 in transforaminal lumbar interbody fusion. Complications associated with posterior and transforaminal lumbar interbody fusion. Vertebral osteolysis after posterior interbody lumbar fusion with recombinant human bone morphogenetic protein 2: a report of five circumstances. Incidental durotomy during lumbar backbone surgical procedure: danger elements and anatomic areas: medical article. Risk elements for unintended durotomy throughout backbone surgical procedure: a multivariate evaluation. Trans-foraminal versus posterior lumbar interbody fusion: comparability of surgical morbidity. The immediately failed lumbar disc surgery: incidence, aetiologies, imaging and management. Symptomatic calcified perineural cyst after use of bone morphogenetic protein in transforaminal lumbar interbody fusion: a case report. Acute epidural lipedema: a novel entity and potential complication of bone morphogenetic protein use in lumbar backbone fusion. Complications of Posterior and Transforaminal Lumbar Interbody Fusion [64] Neidre A, MacNab I. Comparative analysis of perioperative surgical site an infection after minimally invasive versus open posterior/transforaminal lumbar interbody fusion: analysis of hospital billing and discharge information from 5170 sufferers. The distinction of surgical web site infection based on the strategies of lumbar fusion surgery. Prophylactic intraoperative powdered vancomycin and postoperative deep spinal wound infection: 1,512 consecutive surgical circumstances over a 6-year period. Deep vein thrombosis as a end result of migrated graft bone after posterior lumbosacral interbody fusion. Massive postoperative pulmonary embolism in a young woman using oral contraceptives: the worth of a preoperative anesthetic seek the guidance of. A 360-degree fusion with interbody cage and posterior instrumentation provides very high fusion charges. The indications for interbody fusion versus posterolateral fusion alone are still a topic of intense debate by experienced backbone surgeons. Removing the disc not solely takes compression off the dural sac, but additionally removes one of many potential pain turbines of low again ache. Placement of the interbody cage within the anterior one-third of the intervertebral area has the ability to restore a collapsed or kyphotic segment to a more lordotic angle. However, it offers its own disadvantages corresponding to a separate surgical procedure and risk of genitofemoral nerve injury, which shall be mentioned in additional element in one other chapter. Furthermore, the open process permits direct visualization of traversing nerve roots, which we feel is safer. The fascia is dissected off the midline and the paraspinal muscular tissues subperiosteally elevated off the bony elements of the posterior spine with a Cobb elevator. If just one degree is being fused, then it is extremely necessary to not violate uninvolved aspect joints, including the adjoining side joint of the superior degree being fused. This can be prevented by taking a localizing lateral radiograph prior to dissecting previous the sides. The caudal aspect joint of the fusion degree can, nonetheless, safely be uncovered and violated. The transverse processes of each levels must be utterly exposed, as nicely as the intertransverse membrane between them. More laterally, in the neuroforamen, the lateral facet of a hypertrophied superior articular side of the inferior degree can also impinge on the exiting nerve root, along with far lateral disk herniations. The nerve root passes simply medial and then turns out laterally just under the pedicle. Independently of spondylolisthesis and deformity correction, interbody fusion is a useful definitive remedy for recurrent disc herniation. Radiographs (a,b), together with flexion and extension films (c,d), showed a degenerative spondylolisthesis of L4�L5 (continued). Typically, supination of the wrist with the osteotome nonetheless within the side joint will unroof the aspect joint and expose the superior articular facet of the caudad stage. This could be avoided by using a Woodson elevator to palpate the pedicle from throughout the spinal canal and estimate how far inferior the osteotomy can be safely performed. The traversing superior exiting nerve root must be visualized traveling underneath the pedicle above and the traversing inferior nerve root still within the spinal canal should both be seen. Epidural bleeding can be managed with bipolar coagulation beneath direct visualization as nicely as varied anticoagulant agents. The inferior pedicle ought to be skeletonized with a Kerrison rongeur to enhance visualization of the disk area. The disc area can be distracted with a laminar spreader between the spinous processes or the aspect joints. Often the disc house will be coated with a leash of epidural vessels, which ought to be bipolared and swept away.
Pudendal block paralyses the skeletal muscle tissue of perineum and anaesthetizes the pores and skin of perineum allergy treatment for horses order 10 mg zyrtec fast delivery. It additionally results in allergy treatment for dogs 10 mg zyrtec buy with mastercard lack of sensation at the openings of urethra quitting allergy shots discount 10 mg zyrtec mastercard, vagina and anal canal. For a whole anesthesia of the perineal area, the ilioinguinal nerve (which branches into the anterior labial nerves), genitofemoral nerve, and perineal department of the posterior femoral cutaneous nerve are also anesthetized. Vermiform appendix � Pelvic splanchnic nerves are the parasympathetic nerves to supply the pelvic viscera like urinary bladder, uterus and rectum. S2-S3 roots � Pudendal nerve is contributed by the anterior main ramus of S-2, three, 4 in the sacral plexus and supply exterior sphincters of urethra, vagina and anal canal. Leaves pelvis through the lesser sciatic foramen � Pudendal nerve (S2�S4) passes out of the pelvic cavity via the higher sciatic foramen (below the piriformis muscle) and enters the gluteal region. Autonomic nerves � Pelvic ache is carried by the autonomic nervous system: Sympathetic part is carried by lumbar splanchnic nerves (T-12, L1,2) and parasympathetic component is nervi erigentes (S-2,three,4). They come up from the ventral primary ramus of S2,three,four and ascend from the inferior hypogastric plexus via the best and left hypogastric nerves to reach the superior hypogastric plexus. Pelvic Splanchnic nerve � Pelvic viscera are supplied by the inferior hypogastric plexus located by the sides of rectum. It receives postganglionic sympathetic fibres from the superior hypogastric plexus (presacral nerve) and preganglionic parasympathetic fibres from the pelvic splanchnic nerve (S2, S3, and S4). Appendix � Vermiform appendix is half of mid-gut underneath the provision of vagus nerve (not pelvic splanchnic nerves). Inferior a half of vagina � Pudendal nerve provides the constructions in the perineum, together with the opening of vagina. S � 2, 3, four � External anal sphincter is supplied by inferior rectal nerve branch of pudendal nerve. Muscles Pelvic floor consists of a quantity of overlapping sheets of muscular tissues and connective tissues. It closes the pelvic and belly cavities and bear the load of the visceral organs. It management the openings of the gastrointestinal and urogenital tubes that pierce through it. It has two hiatuses: Anteriorly urogenital hiatus through which urethra and vagina move by way of and posteriorly anal hiatus by way of which anal canal passes. Pelvic diaphragm separates the pelvic cavity above from the perineal region under. It lies posterior and deep to the urogenital diaphragm and medial and deep to the ischiorectal fossa. It flexes the anorectal canal during defecation and helps the voluntary management of micturition. It consists of muscle fibers of the levator ani and the coccygeus muscle (covered by the parietal pelvic fascia on their upper and lower aspects), and associated connective tissue which span the world beneath the pelvis. These muscle tissue arise between the symphysis and the ischial spine and converge on the coccyx and the anococcygeal ligament which spans between the tip of the coccyx and the anal hiatus. Right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a slim hole that transmits the urethra, vagina, and anal canal. The levator ani muscle has two components: pubococcygeus (anterior) and iliococcygeus (posterior). Some fibers are inserted into the prostate, urethra, vagina & anorectal junction and named accordingly: puboprostaticus, pubourethralis, pubovaginalis, puborectalis respectively. Ischio-coccygeus (simply referred to as coccygeus) is situated behind the levator ani and frequently tendinous as a lot as muscular, extends from the ischial backbone to the lateral margin of the sacrum and coccyx. Functions of pelvic diaphragm: Excellent help of pelvic viscera (urinary bladder, uterus, rectum and so on. Help in maintenance of continence as part of the urinary, vaginal and anal sphincters. Facilitates birth by resisting the descent of the presenting half, inflicting the foetus to rotate forwards to navigate via the pelvic girdle. Clinical Correlations � Damaged pelvic diaphragm results in prolapse of pelvic viscera and incontinence. Structures attaching to perineal physique: External anal sphincter; Bulbospongiosus muscle; Superficial and deep transverse perineal muscle; Anterior fibers of the levator ani (including puborectalis or pubovaginalis and so forth. Perineal body is a crucial help of pelvic viscera and is crucial for the integrity of the pelvic ground. Perineal physique tear throughout vaginal supply leads to widening of the hole between the anterior free borders of levator ani muscle of each side, thus predisposing the woman to prolapse of pelvic viscera (urinary bladder, uterus, rectum and so on. Table 10: Muscles of perineum Muscle External ter Origin Course and distribution Innervation Main action Constricts anal canal during peristalsis, resisting defecation; supports and flexes perineal body and pelvic ground Male: supports and fixes perineal body/pelvic ground; compresses bulb of penis to expel last drops of urine/semen; assists erection by compressing outflow through deep perineal vein and by pushing blood from bulb into body of penis Female: supports and flexes perineal body/pelvic flooring; "sphincter" of vagina; assists in erection of clitoris (and perhaps bulb of vestibule); compresses greater vestibular gland Maintains erection of penis or clitoris by compressing outflow veins and pushing blood from the root of penis or clitoris into the body of penis or clitoris sphinc- Skin and fascia Passes round lateral elements of Inferior anal (rectal) nerve, a surrounding anus; anal canal, insertion into per- branch of pudendal nerve (S2� coccyx via ano- ineal body S4) coccygeal ligament Male: median rapheon ventral floor of bulb of penis; perineal body Male: surrounds lateral elements Muscular (deep) branch of perof bulb of penis and most ineal nerve, a department of pudenproximal a half of body of penis, dal nerve (S2�S4) inserting into perineal membrane, dorsal side of corpus spongiosum and corpora cavernosa, and fascia of bulb of penis Bulbospongiosus Female: physique perineal Female: passes on each side of decrease vagina, enclosing bulb and higher vestibular gland; inserts into pubic arch and fascia of corpora cavernosa of clitoris Embraces crus of penis of clito- Muscular (deep) branch of perris, inserting onto inferior and ineal nerve, a branch of pudenmedial features of crus and to dal nerve (S2�S4) perineal membrane medial to crus Ischiocavernosus Internal floor of ischiopubic ramus and ischial tuberosity 861 Self Assessment and Review of Anatomy Muscle Superficial transverse perineal muscle Deep transverse perineal muscle Origin Course and distribution Passes along inferior facet of posterior border of perineal membrane to perineal body Passes alongside superior facet of posterior border of perineal membrane to perineal body and external anal sphincter Innervation Main action Supports and flex perineal body/pelvic floor to support abdominopelvic viscera and resist elevated intra stomach strain External urethral (Compressor ure- Surrounds urethra superior to Dorsal nerve of penis or clitoris, sphincter thra portion only) perineal membrane; in males, the terminal department of the puit also ascends anterior aspect dendal nerve (S2�S4) of prostate; in females, some fibers additionally enclose vagina (urethrovaginal sphincter) Compresses urethra to maintain urinary continence; in females, urethrovaginal sphincter portion additionally compresses vagina Bulbospongiosus muscle compress the bulb in the male, impeding venous return from the penis and thereby maintaining Contraction (along with contraction of the ischiocavernosus) constricts the corpus spongiosum, thereby expelling the final Compress the erectile tissue of the vestibular bulbs within the female and constrict the vaginal orifice (vaginal sphincter). Parts of pubococcygeus: pubourethralis, puboprostaticus, pubovaginalis, puborectalis are elements of the diaphragm. Levator ani � Pelvic diaphragm is contributed by levator ani (pubococcygeus and Iliococcygeus) and ischiococcygeus muscular tissues. Pelvis Arterial Supply Internal Pudendal Artery is a branch from the anterior division of internal iliac artery. It leaves the pelvis by the use of the larger sciatic foramen between the piriformis and coccygeus and immediately enters the perineum through the lesser sciatic foramen by hooking across the ischial backbone, accompanied by the pudendal nerve during its course. Branches Table eleven: Arteries of Pelvis Artery Gonadal Testicular Origin Abdominal aorta Course Distribution Descends retroperitoneally; Traverses inguinal canal and Abdominal and/or pelvic ureenter scrotum ter, ovary, and ampullary finish of uterine tube Crosses pelvic brim, descends Abdominal and/or pelvic urein suspensory ligament of ter, ovary, and ampulary end ovary of uterine tube Crosses left common iliac ves- Superior part of rectum sels and descends into pelvis between layers of sigmoid mesocolon Descends close to midline over Inferior lumbar vertebrae, saL4 and L5 vertebrae, sacrum, crum, and coccyx and coccyx Passes medially over pelvic Main blood provide to pelvic brim and descends into pelvic organs, gluteal muscles, and cavity; often types anterior and perineum posterior divisions Passes medially over pelvic Main blood supply to pelvic brim and descends into pelvic organs, gluteal muscle tissue, and cavity; typically types anterior and perineum posterior divisions Runs a short pelvic course, Superior facet of urinary offers off superior vesical arter- bladder and, in some males, ies, then obliterates, changing into ductus deferens (via superior vesical arteries and artery to medial umbilical ligament ductus deferens) Usually multiple; cross to supe- Superior aspect of urinary rior side of urinary bladder bladder; in some males, ductus deferens (via artery to ductus deferens) Runs anterio-inferiorly on ob- Pelvic muscular tissues, nutrient arturator fascia of lateral pelvic tery to ilium, head of femur, wall, exiting pelvis via obtura- and muscles of medial comtor canal partment of thigh Passes subperitoneally in lat- Inferior aspect of male urieral ligament of bladder, giving nary bladder, pelvic a part of rise to prostatic artery and urete; prostate, and seminal occasionally the artery to the glands; often ductus ductus deferens deferens Runs subperitoneally to ductus Ductus deferens deferens Descends on posterolateral as- Prostate and prostatic urepects of prostate thra Runs anatomically in base of Uterus, ligaments of uterus, broad ligament/superior cardi- medial components of uterine tube nal ligament, offers rise to vagi- and ovary, and superior vanal branch, then crosses ureter gina superiorly to attain lateral aspect of uterine cervix Anastomoses Cremasteric artery, artery of ductus deferens Uterine artery through tubal and ovarian branches Middle rectal artery; inferior rectal (internal pudendal) artery Lateral sacral artery (via medial sacral branches) Ovarian Superior rectal Continuation of mesenteric artery inferior Median sacral Posterior side of belly aorta Common iliac artery Internal iliac Anterior division of Internal iliac artery inner iliac Umbilical Anterior division of inner iliac artery (Occasionally the patent part of the umbilical artery) Superior vesical (Patent proximal umbilical artery) Inferior vesical ; Vaginal artery Obturator Inferior epigastric (via pubic branch); umbilical artery Inferior vesical Superior vesical artery Artery to ductus (Superior or inferior vesical deferens artery) Prostatic branches (Inferior vesical artery) Uterine Testicular artery; cremasteric artery Deep perineal (internal pudendal) Ovarian artery (via tubal and ovarian branches); vaginal artery 863 Contd. Obturator artery � Inferior epigastric artery is a department of external (not internal) iliac artery. Anterior division of internal iliac � Anterior division of internal iliac artery provides the inner pudendal artery which accompanies pudendal nerve within the pudendal canal and provide the perineum region. Middle rectal artery � Vas deferens is often derived from the superior vesical artery, and occasionally from the inferior vesical artery, both branches of the internal iliac artery. Inferior epigastric � Accessory obturator artery is the pubic department of inferior epigastric artery, which itself is given by external iliac artery. Venous Drainage Pelvic Venous Plexus It lies within the minor (true) pelvic cavity and is shaped by intercommunicating veins surrounding the pelvic viscera and include the rectal venous plexus, vesical venous plexus, prostatic venous plexus, uterine venous plexus, and vaginal venous plexus. Lymphatics drain by way of the superficial inguinal lymph nodes, which obtain lymph from the lower stomach wall, buttocks, these lymph nodes have efferent vessels that drain primarily into the external iliac nodes and in the end to the lumbar Lymphatics from the glans penis (or clitoris) and labium minus pass to the deep inguinal and external iliac nodes. The lymphatics follow the inner iliac vessels to the inner iliac nodes to the common iliac nodes and subsequently to Internal iliac nodes obtain lymph from the upper part of vagina and other pelvic organs, they usually drain into the common Lymph from the uppermost a half of the rectum drains alongside the superior rectal vessels, inferior mesenteric nodes, and then Lymph from the testis and epididymis or ovary drains alongside the gonadal vessels immediately into the aortic nodes. Lymph vessels from the ovary, uterine tube, and fundus comply with the ovarian artery and drain into the para-aortic nodes. Lymph vessels from the uterine body and cervix and bladder drain into the inner and exterior iliac nodes. Lymphatic Drainage of buildings of pelvis and perineum penis, scrotum, labium majus, and decrease components of the vagina and anal canal. Penile urethra � Lymphatics from the penile urethra (and glans penis) primarily run in course of deep inguinal lymph nodes. Deep inguinal � Distal spongy urethra and the glans penis drain into the deep inguinal lymph nodes of Cloquet and Rosenmuller. Some lymphatics might end in the superficial inguinal/ exterior iliac lymph nodes as nicely. Lymphatic Drainage - Females Table 14: Lymphatic drainage of the female genitalia Structure Vulva Labia, clitoris, and perineum Perineum and decrease labia majora Clitoris Superficial inguinal nodes Rectal lymphatic plexus Superficial inguinal nodes Direct to deep inguinal nodes Direct to inner iliac nodes Internal and external iliac nodes Internal iliac nodes Superficial inguinal nodes Para-aortic nodes Superficial inguinal nodes External iliac nodes Internal iliac nodes Obturator nodes Para-aortic nodes Internal iliac nodes Superficial inguinal nodes Para-aortic nodes Nodes Vagina Upper vagina Mid-vagina Lower vagina Uterus Fundus Isthmus of tube and round ligament Body of uterus, including cervix Uterine (Fallopian) tubes 868 Ovaries Pelvis Male Reproductive System Male reproductive system is described in chapter 9-Abdomen. They are connected to the lateral pelvic wall by the suspensory ligament of the ovary (a area of the broad ligament), which accommodates the ovarian artery, vein, and nerve. The blood vessels, lymphatics, and nerves cross over the pelvic inlet, cross the exterior iliac vessels, and then enter the suspensory ligament of the ovary (lateral finish of broad ligament) and at last enter the hilum of ovary by way of the mesovarium. In younger girls, the outermost portion of the cortex is clean, has a boring white floor (tunica albuginea). There are numerous arteries and veins within the medulla and a small number of clean muscle fibers. Behind the ovarian fossa are retroperitoneal buildings, including the ureter, inside iliac vessels, obturator vessels and nerve, and the origin of the uterine artery. Posterior border of ovary is free and faces the peritoneum, which overlies the higher part of the inner iliac artery and vein, and the ureter.